The technology uses both light and sound to track increasing levels of fibrosis in donated kidneys.
ENO HYSI AND DARREN A. YUEN, ST. MICHAEL’S HOSPITAL; AND MICHAEL C. KOLIOS, RYERSON UNIVERSITY
Chronic kidney disease is a condition that causes the gradual loss of kidney function over a period of months to years. The prevalence of the disease is worsened by the alarming rise of diabetes and hypertension, two of the most common causes of renal failure. The goal of most therapies is to merely slow the progression of the disease. Fortunately, a modern technology called photoacoustic imaging, involving the use of both light and sound, is helping to assess the most efficient treatment for chronic kidney disease: kidney transplantation.
Courtesy of iStock.com/MohammedHaneefaNizamudeen.
Historically, as kidney disease progresses, renal replacement therapy is implemented, in which dialysis is used in attempt to mimic the blood filtration function of the kidneys. Unfortunately, patients with chronic kidney disease experience reduced quality of life, frequent and prolonged hospitalizations, and a significantly higher risk of death. The costs associated with kidney disease care are significant. Each year, Canada spends 40 billion CAD ($31.2 billion) to manage patients with kidney failure1.
Finding healthy transplants
Transplantation has revolutionized treatment for kidney failure, improving both life span and quality of life for transplant recipients. However, with the rapid rise of chronic kidney disease over time, the supply of kidney transplants has failed to keep pace with the growing demand, according to the Kidney Foundation of Canada. Nearly two-thirds of donations come from deceased donors, compared to the number received from living donors. This results in long wait lists because several years may pass before an organ from a deceased donor becomes available1. As patients wait for a new kidney, many become too ill to safely undergo transplantation.
Recognizing the dire need for kidney transplants, physicians have expanded the donor pool by accepting more kidneys from sicker and older donors. Some of these kidneys have donor-derived disease, which can manifest as preexisting scarring, otherwise known as fibrosis. Fibrosis of the renal cortex (the outer part of the kidney) destroys the glomerular capillaries responsible for blood filtration, partially through a buildup of the extracellular matrix2. The core component of this matrix is collagen, a protein that contributes to significant renal dysfunction by replacing the kidney tissue with scar tissue.
The loss of microvasculature leads to hypoxia, which causes the release of profibrotic signals that further augment fibrosis. The fibrotic burden present in donated kidneys is a useful predictor of the long-term transplantation outcomes. The most fibrotic kidney transplants tend to function for a shorter period of time3.
Assessing kidney quality
Donor kidney assessment primarily relies on examinations of donor features such as age, serum creatinine levels, and history of hypertension, diabetes, and vascular disease. While these clinical features are easy to assess, such examinations are surrogate measures that fail to directly ascertain the actual degree of injury in the donor organs. Thus, they lack both sensitivity and specificity in quantifying the transplant’s fibrotic burden, a hurdle that modern optical technology may clear.
Donor kidney biopsy, which is performed at the time of retrieval or transplant, offers the possibility of direct pathologic assessment of fibrosis. However, several major limitations have hindered the potential predictive utility of this test. Chief among these is the undersampling of renal tissue, because the typical biopsy examines less than 1% of the kidney. Since fibrosis can be highly localized, biopsies are subject to sampling bias and cannot assess the fibrosis burden of the whole organ.
Another major limitation is the time required to analyze the biopsy. Extensive sample preparation is required. These processes obliviate the real-world value of biopsies because clinicians do not receive a full, timely assessment of biopsy fibrotic burden when deciding whether to accept a kidney for transplantation. Given the importance of fibrosis to the progression of chronic kidney disease and as a predictor of renal outcomes, there is an obvious need for a noninvasive method that can safely and accurately assess renal fibrotic injury.
Photoacoustic imaging
One of the most recent exciting developments in renal medical imaging involves the combination of light (photo) and sound (acoustic) technologies. Photoacoustic (PA) imaging is a hybrid modality that combines the high resolution of ultrasound imaging with the high contrast provided by optical imaging4. The technique depends on generating acoustic signals from the thermoelastic expansion of tissue in response to the absorption of laser irradiation (Figure 1).
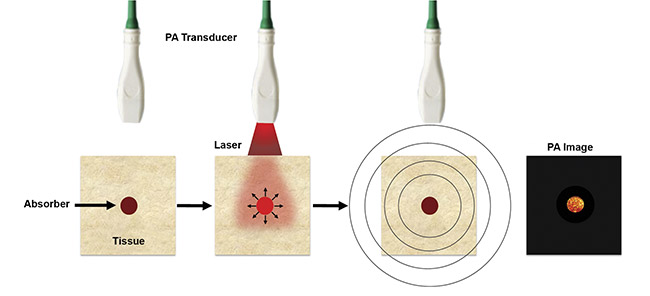
Figure 1. An illustration of photoacoustic (PA) imaging. Adapted with permission from Reference 5.
Fortuitously, many biological tissues and media selectively absorb optical wavelengths in the near-infrared window, where the water absorption is lowest, permitting maximal penetration of light. Generating PA signals depends on the concentration of the chromophore of interest (e.g., hemoglobin, melanin, lipids, collagen, etc.) and its spatial distribution.
Multiwavelength PA imaging enables the acquisition of structural and functional information of chromophores of interest across multiple biological length scales, from organelles up to whole organs5. This is achieved by spectrally unmixing the contributions of each absorber of interest, by taking into account the absorber’s amplitude as a function of illumination wavelength. The most clinically effective application to date for PA imaging has involved using the technology to map the two states of hemoglobin — oxygenated and deoxygenated — to compute the oxygen saturation of blood in normal tissue and in diseased tissue, such as tumors. Using the same hand-held transducers that are used for ultrasound imaging enables simultaneous acquisitions of the anatomy and physiology of the target.
Illuminating fibrosis
PA imaging is well suited for studying the buildup of fibrosis because the technique can detect the spectral signatures of the fibrotic buildup. The kidneys are composed of two dominant chromophores that contribute to the PA signal: blood (in the form of oxygenated and deoxygenated hemoglobin) and collagen (the core component of fibrosis). Because donated kidneys are first examined outside of the body, light penetration is not as limited as with in vivo inspection, allowing for more effective imaging of the organs. Most importantly, through spectral unmixing, clinicians can directly measure the presence of collagen inside kidneys by separating collagen’s contribution to the spectrum from that of blood6.
A mouse model of renal fibrosis was used to test a spectral unmixing algorithm. Fibrosis was induced by clamping the left ureter of each kidney — a procedure known as a unilateral ureteral obstruction, or UUO — for either seven or 14 days to increase the fibrotic burden in the kidney. As shown in Figure 2, the PA maps of the collagen buildup reveal increasing levels of fibrosis by 14 days post-UUO surgery. This is also observed in histology images of fibrosis that were acquired from the same kidney.
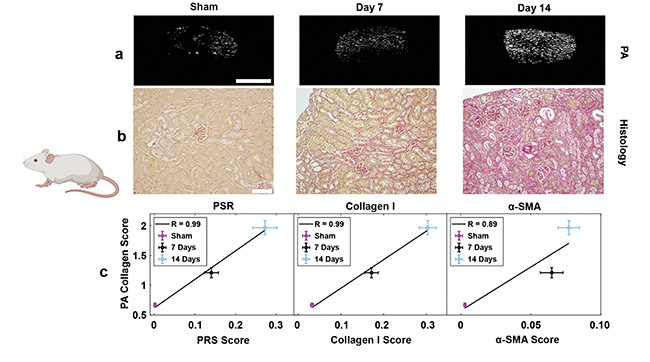
Figure 2. Detecting kidney fibrosis in preclinical mouse models. Collagen maps of fibrosis generated for PA imaging (a) and picrosirius red (PSR) histology (b) as a function of days post-UUO (unilateral ureteral obstruction) surgery. Validation of the PA estimates of collagen against various gold-standard histological scores (c). PA scale bar = 2 mm; histology scale bar = 100 µm. SMA: smooth muscle actin. Adapted with permission from Reference 5.
The agreement of the PA measurement results with those from multiple histological stains validates the algorithm and demonstrates its capabilities to accurately detect fibrosis in mouse kidneys, paving the way toward performing these measurements in donated organs.
Mouse kidneys are significantly smaller than human kidneys. To demonstrate the clinical utility of the algorithm, its performance was tested on pig kidneys, which are similar in size to those of humans. Also tested was the impact of imaging temperature on the PA-based collagen estimates, because kidneys are kept in a saline solution at 4 °C before the transplantation. The results in Figure 3 show that it is possible to scan across the organ and obtain nearly identical collagen estimates at both 4 and 37 °C. These results demonstrate that the fibrotic burden in pig kidneys can be measured in a clinically relevant imaging setting that closely mimics human kidney transplantation.
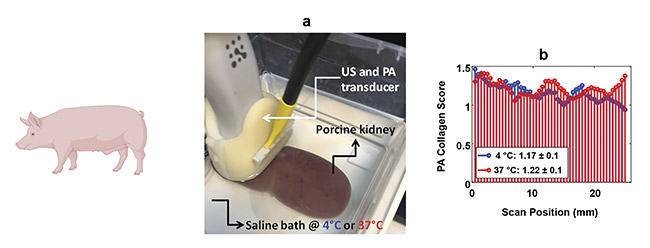
Figure 3. PA imaging can quantify collagen in clinically relevant temperatures. A photograph of the imaging setup (a). PA collagen estimates at two temperatures across multiple scan locations within the kidney (b). US: ultrasound. Adapted with permission from Reference 5.
Lastly, the accuracy of the algorithm was tested on whole human kidneys from a deceased donor that were not suitable for transplant. A high-resolution scan
of the entire kidney takes less than
15 min, although its fibrotic burden can be captured with two-dimensional scans in under 2 min. Figure 4 shows that this technique is capable of accurately measuring collagen on human kidneys that have varying degrees of fibrosis. Since the kidneys are ex vivo, it is possible to sample the entire volume of their cortex by exposing both sides to the transducer. This allows PA imaging to capture the spatial heterogeneity of fibrosis that exists within nearly all of the cortex.
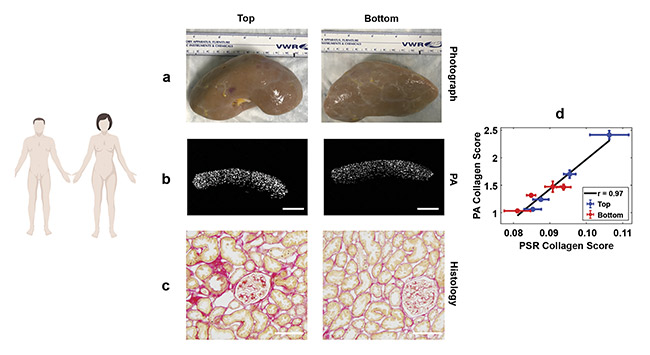
Figure 4. PA imaging of human kidney fibrosis. Photographs (a), PA collagen maps (b), and histology collagen maps (c) extracted from both sides of a whole human kidney. Correlation between PA and histology scores of fibrosis (d). PA scale bar = 2 mm; histology scale bar = 100 µm. PSR: picrosirius red. Adapted with permission from Reference 5.
Clinical impact
Developing a noninvasive kidney fibrosis imaging technique could have significant implications for the clinical assessment of donor kidney suitability. Current kidney transplant allocation methods are problematic, leading to chronically damaged kidneys with shorter life spans often being transplanted into young recipients who need the longest-lasting kidneys. Similarly, uninjured kidneys are sometimes transplanted into elderly patients whose expected life spans are shorter than those of the kidneys.
By providing an accurate assessment of the fibrotic burden in potential human donor kidneys, PA imaging, together with the spectral unmixing algorithm, could enable a better selection of kidneys for transplantation, addressing an important clinical problem for which no solution currently exists. In the long term, these techniques could enhance transplant kidney allocation by enabling clinicians to reject chronically damaged kidneys and to identify functional kidneys that would have otherwise been discarded.
Meet the authors
Eno Hysi, Ph.D., is a Banting and KRESCENT Fellow who works at Toronto’s St. Michael’s Hospital in the Division of Nephrology and in the Keenan Research Centre for Biomedical Science, part of the Li Ka Shing Knowledge Institute. He is interested in the clinical translation of photoacoustic imaging technologies; email: [email protected].
Darren A. Yuen, M.D., Ph.D., is a nephrologist and clinician-scientist at St. Michael’s Hospital and an assistant professor at the University of Toronto. His clinical and research career has been devoted to the development of novel treatments and diagnostic tests for fibrosis, a common injury pathway that is activated by nearly all chronic diseases; email: [email protected].
Michael C. Kolios, Ph.D., is a professor in the Department of Physics at Ryerson University in Toronto and the associate dean of science, research, and graduate studies in the Faculty of Science. His research focuses on the use of ultrasound and optics in the biomedical sciences; email: [email protected].
References
1. Canadian Institute for Health Information (CIHI) (2019). Canadian Organ Replacement Register Metadata (CORR), Treatment of end-stage organ failure in Canada,
www.cihi.ca/en/canadian-organ-replacement-register-metadata-corr.
2. G. Leung et al. (2017). Could MRI be used to image kidney fibrosis? A review of recent advances and remaining barriers. Clin J Am Soc Nephrol, Vol. 12, Issue 6, pp. 1019-1028.
3. A. Srivastava et al. (2018). The prognostic value of histopathologic lesions in native kidney biopsy specimens: results from the Boston Kidney Biopsy Cohort study. J Am Soc Nephrol, Vol. 29, Issue 8, pp. 2213-2224.
4. T. Vu et al. (2019). Listening to tissues with new light: recent technological advances in photoacoustic imaging. J Opt, Vol. 21, Issue 10, www.doi:10.1088/2040-8986/ab3b1a.
5. L.V. Wang and S. Hu (2012). Photoacoustic tomography: in vivo imaging from organelles to organs. Science, Vol. 335, No. 6075, pp. 1458-1462.
6. E. Hysi et al. (2020). Photoacoustic imaging of kidney fibrosis for assessing pretransplant organ quality. JCI Insight, Vol. 5, No. 10.