With the right precautions, lasers can be implemented safely in a medical setting
Vangie Dennis, Gwinnett Medical Center-Duluth, Duluth, Ga.
When lasers are introduced into a health care environment – whether a hospital, surgery center or physician’s office – professionals must be prepared to address safety issues concerning both the staff and patient. All lasers present hazards to the individuals operating them, to patients and to anyone present in the activation area.

Lasers can cause blindness, skin burns, electrocution and fires, making safety a concern for all.
The Code of Federal Regulations’ Performance Standards for Light-Emitting Products provides specifications for manufacturers of medical laser systems. All medical lasers are regulated by the FDA under the Medical Device Amendments to the Food and Drug Act, which applies primarily to laser manufacturers. These regulations are enforced by the National Center for Devices and Radiological Health. The FDA regulates more than 250 types of lasers, including those intended for medical and surgical use. Federal guidelines require manufacturers to classify the medical laser system based on its capacity to damage the eyes and skin. Because of their potential hazards, medical lasers are categorized by the FDA as medical devices class III, subdivision class 4 (See Box 1).
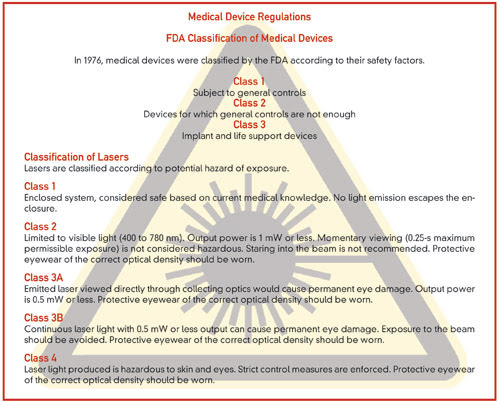
Box 1. The FDA classifies lasers according to their potential hazards.
The American National Standards Institute (ANSI) is a voluntary organization of experts – including manufacturers and consumers as well as government agencies and scientific, technical and professional organizations – that determines consensus of industry standards in the technical fields. Federal legislation and state laser safety regulations, along with professional and advisory standards, are based on the ANSI standard.
The Occupational Safety and Health Administration (OSHA) focuses primarily on the safety of health care workers. Although OSHA does not have specific regulations governing laser safety in health care facilities, it is the agency that can enforce the ANSI standards. OSHA can cite violations under the general duty clause if the level of compliance is not satisfactory.
The number of states enacting medical laser safety legislation is increasing, reflecting the growing concern. Only the FDA and individual states have passed legislation. All other guidelines, which are based on the ANSI Z136.3 practices, are simply recommendations. However, the regulations that do exist present health care personnel with a complex set of standards.
Standards and practice
Minimizing the health hazards associated with the use of surgical laser systems requires the adoption of appropriate safety standards and policies that are relevant to the specific situation. It is imperative that, for the protection of patients, physicians, nurses and other medical personnel, everyone involved with medical lasers understands how to safely manage each type of device. Before a laser is used in the clinic, written policies and procedures regarding authority and accountability should be established.
Operational guidelines should require that the switch controlling laser energy, whether a foot pedal or a finger trigger, be guarded to prevent accidental activation. This precaution may necessitate that the individual controlling the delivery device have access to only one foot pedal.1 Accessory attachments to lasers also must be compatible with safety guidelines. On operating microscopes, these include laser filters that protect the operator at the binocular and accessory viewing tubes.
To prevent accidental discharge, a laser should be in standby mode when it is on but not being fired, or when the user is no longer in control of the delivery device. When not in use, the laser should be stored and/or disabled to prevent its inadvertent activation by unauthorized personnel.
Instruments positioned near the laser should be nonreflecting (dull, anodized or matte-finished) to defocus or disperse the beam.2 Appropriate backstops or guards should be used to prevent the beam from striking nontargeted tissues.
The nominal hazard zone (NHZ) is the space in which the level of the direct, reflected or scattered radiation from normal laser operation exceeds the applicable maximum permissible exposure.3 When determining the NHZ, one should take into consideration information gathered from the manufacturer’s labeling, radiation transmission of the beam and the potential for equipment failure. The NHZ usually is contained within the room but may extend beyond open doors or transparent windows, depending on the type of laser involved.
For this reason, the use of windows and viewing areas must be limited. Depending on the laser used, additional safety controls may include restricting traffic or closing doors and covering windows with applicable filters or barriers. Screens, curtains or a blocking barrier may be placed near entryways to avert laser radiation.
The appropriate warning signs posted at every entryway into the laser treatment controlled area should define the NHZ. The symbols and wording should be specific for the type of laser in use and should conform to the ANSI standards for health care facilities.
Only people authorized by the laser safety officer should be in the vicinity of the NHZ, and only those who have been authorized and trained by the facility’s laser safety officer to perform specific tasks may operate the laser.
To avoid inadvertent exposure to laser hazards, all health care personnel in the vicinity of the NHZ should be trained to implement all safety precautions. All personnel within the zone, including the patient, should use appropriate personal protective equipment. Preventative maintenance on the laser should be done every six months.4

Users must take precautions to prevent lasers from being fired accidentally as well as to minimize stray beams.
Protective equipment
The eye is the organ most susceptible to laser injury. The optics of the eye can concentrate and focus laser light, at wavelengths ranging from 400 to 1400 nm, on the retina, which increases the potential ocular hazard. Ultraviolet and far-infrared wavelength regions (outside the 400- to 1400-nm spectrum) produce principally corneal effects. Also, laser radiation at certain wavelengths may damage the eye’s lens.5
Appropriate laser safety eyewear filters out the hazardous radiation wavelengths and offers protection from the scattered, diffused and reflected laser beams that can cause eye injuries. Laser-protective eyewear may include goggles, face shields, prescription glasses with special filters or coatings, and corneal shields.

The eye is the organ most susceptible to laser injury.
When the patient’s eyes and eyelids are in the NHZ, they should be protected with equipment such as wet eye pads or laser-specific eye shields. Corneal shields may be necessary when goggles or glasses interfere with treatment.
Depending on the laser being used, surgical gloves, tightly woven fabrics or flame-retardant material may provide skin protection. Exposed tissue near the operating site may be covered with saline- or water-saturated fire/flame-retardant materials (e.g., towels, sponges, drapes, fabrics), which must remain moist to absorb or disperse the beam’s energy.

Electrocution is a leading cause of laser-related deaths.
Electrical hazards
Lasers contain high-voltage electrical circuits with the potential to shock, electrocute or cause fires. Hazards such as these are some of the leading causes of laser-related injury and death. Damaged electrical cords, faulty grounding, lack of compliance with training programs, and inadequate or inappropriate use of Lockout/Tagout procedures can be avoided by adherence to the facility’s standard operating procedures. Visual inspection of the laser – including the accessory equipment, gas supply, and plumbing and delivery systems – as well as sterile draping6 before use may prevent injuries. Observing general safety practices (e.g., no fluids placed on or near lasers, no use of extension cords to power lasers) also is important.
Personnel should be aware of the items that could cause a fire, burns or explosions. These include surgical drapes, endotracheal tubes, paper or gauze materials, gases (e.g., oxygen, methane, anesthetic gases), and flammable liquids or ointments (e.g., skin-preparation solutions, oil-based lubricants).7 Water or saline and fire extinguishers should be readily available wherever lasers are used.
Laser plume
Vaporization of tissues may release toxic substances (e.g., acetone, isopropanol, toluene, formaldehyde, metal fumes and cyanide), including carcinogens and viruses, from the cells. This laser plume contains water, carbonized particles, mutated DNA and intact cells. At certain concentrations, it may cause upper respiratory tract or ocular irritation and emit unpleasant odors. The substances in the plume should not be inhaled, so some type of smoke evacuation system must be used.8 Removal of the plume also will enhance the visualization of the surgical/treatment site and may prevent reflection of the laser beam.
Multiple controls should be implemented to minimize smoke plume inhalation. Devices for this purpose may include high-filtration masks, wall suction units with in-line filters or smoke evacuators. High-filtration masks, which should fit tightly and filter particles as small as 0.1 μm, should be used in conjunction with other controls and not as a sole means of protection.9 Wall suction systems may be used when generation of a minimal amount of plume is expected, such as in laparoscopic cases. Wall units produce low suction rates and are designed for fluids; to collect particulate matter, an in-line filter should be used. A mechanical smoke evacuator or suction with a high-efficiency filter should be used to eliminate a large amount of laser plume. (When handling the contaminated filters, standard precautions should be taken, such as using gloves and a mask.) These systems should be turned on at the same time the laser is activated and placed as close as possible to the laser site.
Regardless of the setting – a small clinic, a doctor’s office or a large hospital – the presence of laser equipment creates a need for unique control measures and for the development and implementation of safety practices. Taking precautions is not the responsibility of one individual but the obligation and duty of everyone involved in the laser surgery process. Any health care provider could be in the vicinity of the NHZ and thus should be educated appropriately on maintaining a protected environment for patient care. A laser safety program that is developed according to the ANSI Z136 series and implemented properly should safeguard all personnel. When everyone knows the fundamentals of maintaining a laser-safe environment, the risk of accidents resulting from ignorance of, or noncompliance with, policy is greatly reduced.
References
1. American National Standards Institute (2007). American National Standard for Safe Use of Lasers in Health Care Facilities Z136.3, 31.
2. Phillips, Nancymarie (2004). Berry & Kohn’s Operating Room Technique. 10th ed. Mosby-Year Book Inc., 355.
3. American National Standards Institute (2007). American National Standard for Safe Use of Lasers in Health Care Facilities Z136.3, 5.
4. Laser Institute of America (1997). Guide to Medical Laser Safety, 33.
5. Laser Institute of America (1997). Guide to Medical Laser Safety, 15.
6. Laser Institute of America (1997). Guide to Medical Laser Safety, 32.
7. American National Standards Institute. American National Standard for Safe Use of Lasers in Health Care Facilities Z136.3, 31.
8. American National Standards Institute (2007). American National Standard for Safe Use of Lasers in Health Care Facilities Z136.3, 15-16.
9. Phillips, Nancymarie (2004). Berry & Kohn’s Operating Room Technique. 10th ed. Mosby-Year Book Inc., 354.
Meet the author
Vangie Dennis is a certified medical laser safety officer and teaches medical laser safety for the Laser Institute of America. She also is the clinical manager for procedural nursing for Gwinnett Medical Center-Duluth in Georgia; e-mail: [email protected].