Ever more reliable and compact, medical lasers continue to drive innovative treatments in ophthalmology, dentistry, dermatology, and neurology.
Medical lasers have been used for decades in surgical contexts.
In recent years, the development of compact, easy-to-use, and often self-contained modules has opened doors for new or enhanced procedures in ophthalmology, dentistry, dermatology, and neurosurgery to improve patient quality of life. Flexibility in the technologies that power and focus medical lasers has changed the lasers’ primary use from cutting and removing — essentially as a high-tech scalpel — to minimally invasive cleaning and reinvigoration of damaged areas in the body.
These developments have been made possible by improvements in the understanding of various wavelengths and pulse durations, and the wide variety of results that each can produce, depending on what tissue and depth is being targeted.

iStock.com/FG Trade
These technological advancements — along with improvements in reliability, footprint, cost, and usability — have helped to broaden the adoption of medical lasers in all of the disciplines mentioned above. But demand-side factors are also driving growth.
Practitioners in ophthalmology, for example, are seeking innovative laser-based solutions to correct and improve vision, according to Matthias Schulze, director of marketing of OEM components and instrumentation at Coherent Inc. This trend is fueled, in turn, by larger trends, such as the growing demand for corrective eye surgeries from an aging population, as well as from increasingly affluent customers in the Asian marketplace.
An eye for laser treatment
Laser eye treatments, such as cataract and refractive corneal surgery, continue to command the vast majority of the medical laser market, said Francois Guillot, medical segment leader at Amplitude Laser Group SAS.
For cataract surgery, the favored lasers are femtosecond sources operating at 1030 nm, a wavelength that can safely penetrate transparent tissue and, in the process, perform corneal incisions and lens fragmentation. Nd:YAG lasers emitting at 1064 nm are often used post-surgery to cut a small hole in the lens capsule to allow the flow of aqueous fluid within the eye chamber. This helps to prevent secondary cataracts, which can develop a few months after cataract surgery. Secondary cataracts occur when protein starts to accumulate on the posterior lens capsule of the eye.
Femtosecond lasers are also used for refractive corneal surgery, where they reshape the cornea by removing a portion of the tissue, and then the resulting flap is folded back into place. Lasik surgery is one of the most common types of this treatment. Alternatively, excimer lasers at 193 nm that produce a cool beam of ultraviolet light can be used to disrupt chemical bonds in the corneal tissue without damaging the surrounding area.
According to Guillot, the femtosecond lasers produced by Amplitude have undergone a transformation driven, in part, by lessons learned from the proliferation of the technology in industrial settings. In the last 15 years, the reliability of lasers has improved, along with the ability to produce them at high volume. These advancements have attracted medical users who are looking for technology that is small, compact, and easy to use, Guillot said. The trend toward easier manufacturability has also positioned femtosecond laser technology to meet growing demand for these instruments in medical applications.
“The growth of the femtosecond laser market is expected to reach 10% per year for the foreseeable future,” Guillot said. “Part of that has to do with the increasing age of the population in wealthy countries. For example, China has been getting into cataract treatment more recently, but as the country has gotten richer, so has the demand.”
No more drills
Laser technology is also enhancing certain dental procedures. Scientists and engineers at BIOLASE Inc. and other companies have developed specially designed erbium-based lasers capable of treating both hard and soft tissue in a variety of surgical applications in dentistry. With the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) both noting a rising number of adults and children affected by periodontal disease, the timing for this innovation couldn’t be better.

Clinicians track the progress of a laser dental treatment. Courtesy of BIOLASE.
“The reality is the bacteria in gum disease is carried to all parts of our bodies, all the time, and can affect the heart and other organs, and has been connected to everything from diabetes to low-birth-weight babies,” said William Brown, vice president of innovation and business development at BIOLASE. “But when it comes to surgery, no one wants pain, bleeding, and sutures, and they want quicker recovery times.”
Laser technology is helping to deliver these improvements. Brown pointed to recent research led by scientists at the Houston-based McGuire Institute that validated the use of an Er,Cr:YSGG laser as an effective alternative for the management of periodontitis1. The laser sources applied in the studies delivered 60-µs pulses at a frequency of 50 Hz. The researchers found their laser-based approach to be as effective as, but — due to a shorter recovery period — preferable to a traditional minimally invasive surgical technique that involves retracting a specific area of the gums, treating the bone, and suturing the retracted tissue. The study included 53 adults: 29 women and 24 men.
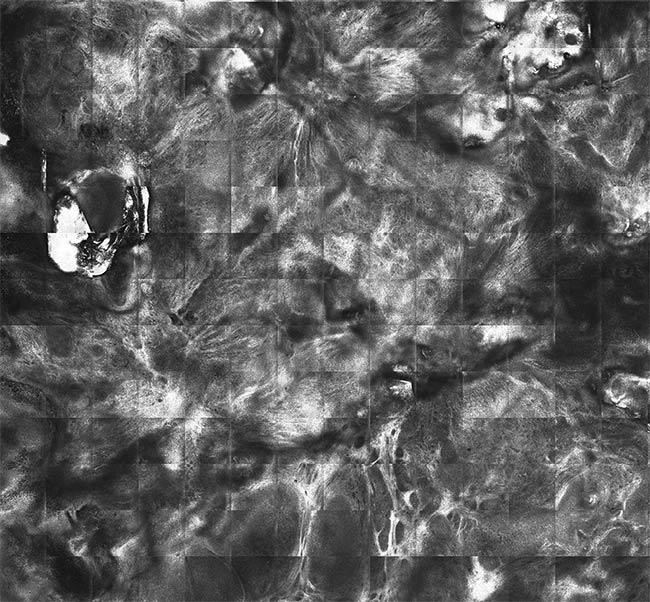

A reflectance confocal microscopy image of basal cell carcinoma prior to treatment with a carbon dioxide laser (top). A reflectance confocal microscopy image of the skin area following treatment of the carcinoma with a laser (bottom), showing that the treatment was able to identify and remove many residual cancer cells on the first pass with the laser. Courtesy of Miguel Cordova and Anthony Rossi.
Brown said that lasers at this or similar wavelengths can also be used to treat the surfaces of failing dental implants, as a favorable alternative to removal and replacement. Samuel Low, chief dental officer at BIOLASE, agreed: “Peri-implantitis — the inflammation of tissue surrounding an implant — is a common problem,” he said. “There are about
3 million implants every year in the U.S., and we believe 10% to 15% of these are lost over time, which can cost thousands of dollars to replace, not counting the inconvenience.”
The erbium-based lasers used for this application have been clinically proven to have no adverse effects on the titanium surface of the implants during the process of removing toxins. In such procedures, Brown said, the beam can be directed through a side-firing tip to treat both the bone and the surface of the implant, without damaging nearby soft tissue.
Brown estimated that 30% of BIOLASE’s sales are to dental specialists.
But he and Low said that laser training is very limited in dentistry. BIOLASE now offers its own training in the use of its laser technology.
“The advantage of lasers in dentistry is that there is very little blood,” Brown said. “My daughter is 30, and she’s never had a drill used on a tooth. That means more patient comfort.”
Lasers get under the skin
Many factors affect the selection of a laser for dermatological procedures, said Dr. Anthony Rossi, a surgeon at Memorial Sloan Kettering Cancer Center and a specialist in the application of laser technology in dermatology. These factors typically depend on the particular application, which may range from cosmetic treatment to Rossi’s specialty, Mohs micrographic surgery and reconstruction — a skin cancer treatment in which thin skin tissue layers are removed in stages and examined microscopically until cancer cells are determined to be no longer present.
Rossi said that the specifications of the laser system also depend on the target within the epidermis, such as water, hemoglobin, or pigment. He said Nd:YAG lasers, for example — with a common wavelength of 1064 nm — are most effective in reaching the vasculature, whereas ablative lasers, such as CO2 or Er:YAG, are effective at destroying tissue via the water chromophore.
Factors such as water and hemoglobin
levels affect how deeply the laser penetrates tissue, which is a consideration when the aim is to treat blood vessels without affecting the skin pigment
(melanin).
Laser selection also influences and is influenced by other technologies that are applied alongside the laser itself.
“When we treat basal cell carcinoma, for example, we use reflectance confocal microscopy (RCM) to provide images
that guide the carbon dioxide laser in the ablation of these cells,” Rossi said. “The RCM is performed with a hand-held device, and this helps increase the effectiveness of the targeting of the laser at the tumor.”
As a recent study demonstrated, when CO2 lasers and RCM were used together on 22 basal cell carcinoma tumor sites in nine patients, RCM was able to increase the precision of treatment, enabling the identification and removal of many residual cancer cells with the first pass of the laser2. In the studies, laser ablation of the skin was conducted with a Lumenis CO2 laser that removed 20 to 30 µm of tissue, at a fluence of 300 to 350 mJ/cm2. No recurrences of the carcinoma have been reported since the study ended over two years ago.
Lasers on the brain
Though the use of lasers in neuroscience and neurosurgery encompasses a small share of the medical laser market, the potential benefits of the instruments are powering future growth.
Optogenetics — an approach that
uses light from a laser to excite specific neurons — is being studied more extensively as technology has progressed and could hold promise as a future treatment
of neurodegenerative conditions such
as Alzheimer’s and Parkinson’s diseases by reactivating certain areas in the brain.
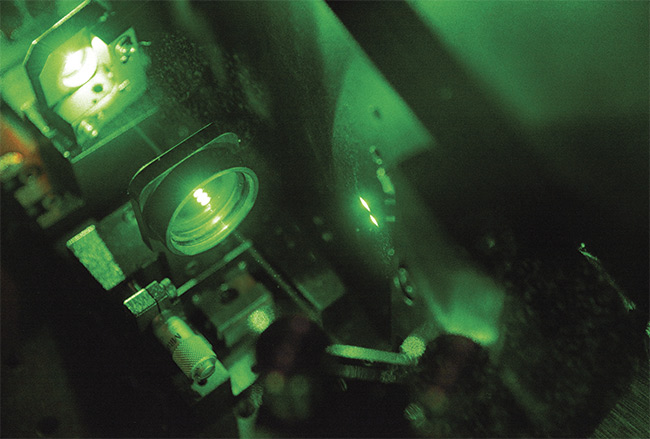
Marco Arrigoni, director of marketing for the scientific segment at Coherent, explained what a typical optogenetic stimulation setup looks like in rodent studies. “The most popular approach is to use a spatial light modulator (SLM) to create a holographic pattern that splits the beam into beamlets, each one addressing
a neuron of choice in a 3D volume in the brain,” he said. “The targeted volume typically encompasses 50 to 300 neurons among the 10,000 to 20,000 occupying a 0.5-mm3 cube of mouse brain tissue.
If you change the SLM pattern, you can then address different neurons.”
Optogenetic probes are manufactured versions of opsins — light-sensitive proteins that bind to membranes and transfer ions following stimulation by specific wavelengths of light. These probes use LEDs for wide-area stimulation and lasers for targeted stimulation. The prescribed wavelength depends on the opsin used.
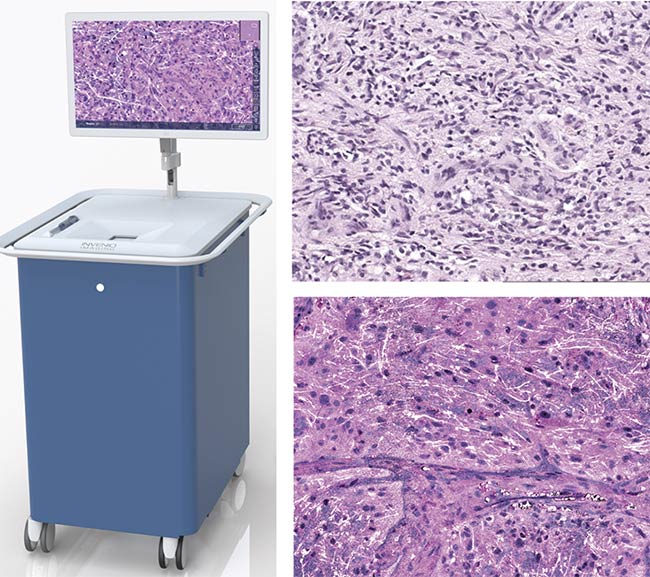
A rendering of the NIO Laser Imaging System developed by Invenio (left). An image captured with traditional H&E stain histology (top right) versus the stimulated Raman histology the system captures (bottom right). Invenio’s system leverages a dual-wavelength fiber laser based on erbium and ytterbium sources to capture 3D color images for neurosurgery without the need for sectioning or dye staining. Courtesy of Invenio.
Arrigoni said optogenetic and other functional probes are based on green fluorescent proteins, which are sensitive to blue light: 480 nm (one photon), 920 to 950 nm (two photons), and 1300 nm (three photons). So-called red-shifted proteins are sensitive to green light: 530 nm (one photon), 1000 to 1200 nm (two photons), and 1700 nm (three photons). Up to this point, he said, three-photon excitation has primarily been used for morphology and calcium imaging.
Currently, most of the advanced forms of optogenetics are done in two photons, at either 1040 or 920 nm. “Lasers are more powerful at 1040 nm than at
920 nm. So, it’s common to use 40 W of power at 1040 nm to address some hundreds of neurons. It looks like an awfully high power, but microscope plus SLM losses are large, and light is flashed for milliseconds and spread on many neurons,” Arrigoni said.
Illuminating the brain
Lasers have also enabled new breakthroughs in neuroimaging, such as the use of stimulated Raman histology, which utilizes laser spectroscopy to identify the chemical composition of a sample. A dual-wavelength fiber laser is used in conjunction with an optical parametric oscillator because the frequencies of erbium- and ytterbium-based sources overlap with the Raman spectra. This method can display a 3D color image without the need for sectioning or dye staining, providing guidance to surgeons while requiring minimal sample preparation.
This is the principle behind a laser imaging system launched in 2015 by Invenio Imaging Inc. that is enabled by solid-state lasers provided by Coherent. Invenio’s system targets applications in neurosurgery and incorporates two lasers — one operating at 790 nm and the other at 1020 nm — to image the margins of a tumor.
“We looked at what the standard of care was, which at this point was a biopsy that involves a sample being wrapped in plastic or frozen and cut into sections, which are then stained,” said Christian Freudiger, Invenio’s co-founder and vice president of R&D. “You can recognize the pattern of cells when you do this, but it is very labor intensive and it can take weeks. Not to mention that with the brain, biopsies aren’t preferred.”
Freudiger said the images created by this two-laser method and often stitched together could provide a neurosurgeon with the information needed to make a real-time decision.
“Brain tumors are very infiltrative, so the images need to be clear enough to provide very specific margins,” he said. “Obviously, when it comes to the brain, a surgeon is going to take a minimalist approach.”
Freudiger acknowledged that Invenio’s ultimate goal, once its technology is established in the medical community, is for the company to be acquired by a bigger producer in the medical laser market.
“That’s probably our most realistic option,” he said. And it echoes a practice that Coherent’s Schulze said is common throughout the laser market.
“We have systems at major cancer centers and we just sold one in Europe, as well,” Freudiger said. “We believe this technology could help simplify treatment for both the doctor and the patient.”
References
1. D. Clem et al. (2021). Comparison of Er,Cr:YSGG laser to minimally invasive surgical technique in the treatment of intrabony defects: six-month results of a multicenter, randomized, controlled study.
J Periodontol, Vol. 92, Issue 4, pp. 496-506.
2. C. Navarrete-Dechent et al. (2019). Reflectance confocal microscopy-guided carbon dioxide laser ablation of low-risk basal cell carcinoma: a prospective study. J Am Acad Dermatol, Vol. 81, Issue 4, pp. 984-988.
Treating Epilepsy with a Lighter Touch
A team of researchers and clinicians at Cornell University has been experimenting with unique ways that pulsed lasers can be employed to reduce, if not eliminate, the effects of seizures on animal subjects1. While human clinical application is likely years away, the researchers were hopeful about the findings that their results have revealed to this point.
They said that an estimated 2.8% of the population (1 out of 26 people in the U.S.) is stricken by either generalized epilepsy (in which an imbalance of excitatory and inhibitory neural connections can induce seizures throughout the brain) or focal epilepsy (in which the imbalance begins in one region of the brain and propagates to larger areas).
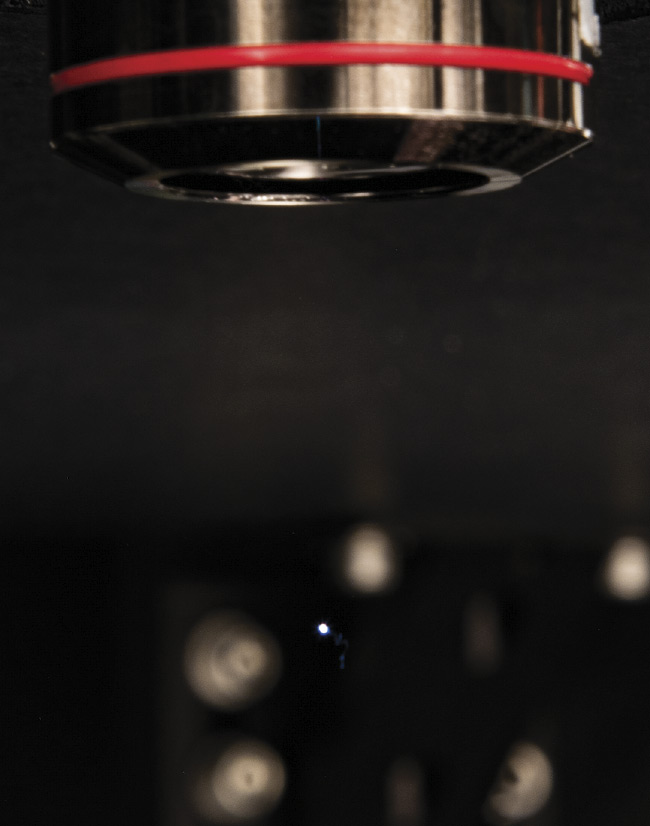
Cornell University researchers used pulses from a Ti:sapphire laser to reduce seizure propagation in rat brains. Courtesy of Seth Lieberman/Cornell University.
The Ti:sapphire laser uses 50-fs pulses at an 800-nm wavelength to create the desired effect in rat brains. Courtesy of Seth Lieberman/Cornell University.
“Now the standard curative treatment for focal epilepsy is resection, which can work well, but it can also produce permanent neurological deficits,” said Chris Schaffer, an associate professor in the Meinig School of Biomedical Engineering at Cornell.
Imaging methods have shown that most seizures spread laterally in specific cortical layers within the brain. Severing just these connections instead of resecting the entire epileptic focus could reduce the neurological deficits of epilepsy surgery. However, cutting subsurface neural connections is not a procedure that can be performed with a mechanical scalpel.
“In our work, we wanted to create a precise laser scalpel and have laser pulses that could cut very sharply, deep within the tissue, without affecting the surrounding tissue,” Schaffer said.
The researchers used a Ti:sapphire laser emitting at 800 nm that generated 50-fs pulses on rat brains to create ~100-µm-wide subsurface cortical incisions in the neocortex. These incisions produced a “box” around a chemically induced epileptic focus that blocked seizure propagation.
Other neural signals entering and leaving the mouse brain cortex — such as the neural signals required to coordinate the action of reaching for pellets or to feel sensations
in the tail — were not interrupted. Laser speckle imaging revealed that blood flow
was not affected in the region incised with the laser.
Utilizing an acutely induced model of seizures, Schaffer’s lab was able to show that all seizure propagation was successfully blocked in one-third of the rats in the study. In other cases, seizure frequency or propagation was reduced. In the ongoing study, the researchers switched to a chronic model of seizures, and the results so far are surprising, they said. Researchers have been able to increase the efficiency of the laser cuts to block upward of 80% of seizure propagation in their subjects for months.
Schaffer credited Theodore Schwartz, a neurosurgeon at Weill Cornell Medicine, with conceiving of a laser-based approach that improved upon the 3-decade-old surgical procedure called multiple subpial transection, which uses a curved needle to produce the interruption of seizure propagation.
Both Schaffer and Seth Lieberman, a doctoral candidate engaged in the research, said that the next step is to seek grant funding to build on their success in animal models and take them one step closer to clinical application.
“We’ve been using an animal model with a flat cortex in our studies to this point, and we are looking to move into a model with a cortex that has folds (gyri) and indentations (sulci), which is more analogous to the human brain,” Lieberman said. “The idea is that we can build a map of how the seizures propagate through the brain and eventually come up with a treatment plan to cut specific lateral connections.”
Reference
1. S. Nagappan et al. (2019). In vivo femto-
second laser subsurface cortical micro-
transections attenuate acute rat focal seizures. Cereb Cortex, Vol. 29, Issue 8, pp. 3415-3426.