Preliminary studies demonstrate that the Er:YAG laser performs a precise urethral incision with minimal thermal damage.
Dr. Nathaniel M. Fried, University of North Carolina at Charlotte, and Dr. John A. Munoz, Manchester Urology Associates
Urethral stricture disease, characterized by a narrowing of the urethra, may develop after trauma, indwelling catheterization, endoscopic urological procedures or radical prostatectomy surgery for prostate cancer. Those with stricture disease may experience obstructive voiding, recurrent urinary tract infections and even urinary retention.
The gold standard for treatment of urethral strictures is open reconstructive surgery of the urethra, or urethroplasty. This procedure has a success rate of approximately 97 percent; however, it is invasive and expensive and can carry with it considerable complications. Minimally invasive therapies include balloon dilation, cold knife incision, electrocautery and Ho:YAG laser ablation. These procedures have success rates that vary from 20 to 80 percent because of a number of factors, including variations in surgical technique and skill, type of stricture, patient postoperative monitoring time and definition of stricture. The most common complication of minimally invasive therapy is a recurrence of the stricture as a result of mechanical or thermal damage caused during the procedure. Studies have shown that multiple dilations or incisions in patients with complicated urethral strictures do not provide any increased benefit, leaving the patients without any effective method of treatment for their incontinence.
A laser that can precisely vaporize or incise the scar tissue at the site of the urethral stricture with minimal peripheral thermal damage to adjacent healthy tissue may produce higher success rates. Because of its precision, the Er:YAG laser is used in the clinic for skin resurfacing and caries removal. The laser’s 2.94-μm wavelength exactly matches a major water absorption peak in tissue, allowing precise tissue ablation with minimal thermal insult to adjacent healthy tissue.
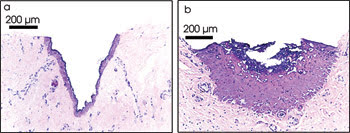
Figure 1. A comparison of laser incision of urethral tissues with the Er:YAG (a) and Ho:YAG (b) lasers shows the purple region at the border of the ablation crater. Undesirable thermal damage to tissue may contribute to delayed wound healing, scarring and stricture recurrence.
Preliminary studies in Nathaniel M. Fried’s laboratory using a scientific Er:YAG laser from Schwartz Electro-Optics of Orlando, Fla., demonstrated that this laser can incise urethral tissue with approximately 20 times less thermal damage than the Ho:YAG, the current laser of choice in urology (Figure 1).1,2 Short-term in vivo studies on pigs also demonstrated that Er:YAG laser incisions in the urethra heal twice as rapidly and with four times less scarring than Ho:YAG laser incisions.3
Recently, studies were initiated using a clinical Er:YAG laser from Sciton Inc. of Palo Alto, Calif., for the precise incision of urethral strictures in patients (Figures 2 and 3).4 From January 2006 to March 2007, five patients were treated in the Davison Laser Center at Elliot Hospital in Manchester, N.H.
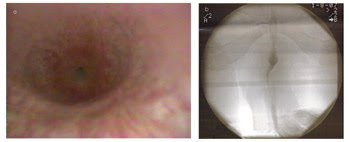
Figure 2. Endoscopic (a) and x-ray (b) images show narrowing of the urethra at the site of the stricture before treatment with the Er:YAG laser.
The Er:YAG laser was modified for use in urology. A fiber optic port replaced the articulated arm typically used, and the temporal pulse structure of the laser was optimized for easy coupling into optical fibers and for more efficient tissue ablation. The laser was operated at a wavelength of 2.94 μm, with pulse energies of 10 to 23 mJ and with pulse repetition rates of 15 to 35 Hz. The laser radiation was delivered through a 2-m-long sapphire optical fiber with a 250-μm core from Photran Inc. of Poway, Calif. A rigid continuous-flow irrigation operating endoscope from Richard Wolf Medical Instruments Corp. of Vernon Hills, Ill., with a 20° viewing angle and a 5 French (1.7 mm) working channel was used for the procedures. Both the Er:YAG laser and the fiber delivery system had previously received FDA clearance for use in soft tissue procedures in urology.
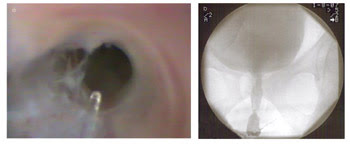
Figure 3. This endoscopic image shows urethral stricture during treatment with the Erbium:YAG laser and sapphire optical fiber (a), and x-ray image of the urethra after treatment (b).
The success of the procedure was evaluated by comparing the patients’ rate of urination before and after surgery. Preoperative average flow rates ranged from 2.2 to 5.3 ml/s. Four patients experienced a successful ablation of scar tissue and improved flow rates with no observed side effects. Postoperative average flow rates measured 9.2 to 11.7 ml/s during short-term follow-up in the patients treated successfully with the Er:YAG laser. One challenging case was presented by a patient who had had multiple recurring urethral strictures. Although the laser procedure was not effective in this instance, the patient was treated safely and without complications.
This is the first reported case study using the Er:YAG laser to treat urology patients. All five were treated safely with no complications resulting from the procedure. Based on these results, a larger case study is planned to determine the long-term efficacy of the Er:YAG laser for treating urethral strictures.
Meet the authors
Nathaniel M. Fried is an assistant professor in the department of physics and optical science at the University of North Carolina at Charlotte; Dr. John A. Munoz is a urologist with Manchester Urology Associates in Manchester, N.H.
References
1. N.M. Fried (2001). Potential applications of the Erbium:YAG laser in endourology. J Endourol, Vol. 1, pp. 889-894.
2. N.M. Fried et al (2003). Optimization of the Erbium:YAG laser for precise incision of ureteral and urethral tissues: in vitro and in vivo results. Lasers Surg Med, Vol. 33, pp. 108-114.
3. I.M. Varkarakis et al (2005). Comparison of Erbium:YAG and Holmium:YAG lasers for incision of the urethra and bladder neck in a chronic porcine model. Urology, Vol. 65, pp. 191-195.
4. J.A. Munoz et al (2007). Erbium:YAG laser incision of urethral strictures: early clinical results. Photonic Therapeutics and Diagnostics III (SPIE, San Jose, CA). Vol. 6424 (1F), pp. 1-4