Recent advances can reduce the size and cost of devices to simplify workflows and increase accessibility.
CELINE CANAL AND ANDREAS KOHL, QUANTEL LASER
Through hundreds of publications and conference papers each year, photoacoustic imaging (PAI) has been shown to have potential for early detection of afflictions such as skin and thyroid cancer, cardiovascular disease, and arthritis. The noninvasive technique combines pulsed laser light for the excitation of tissues with an ultrasound transducer as a receptor. PAI penetrates much deeper than purely optical imaging technologies such as optical coherence tomography. It also offers far greater specificity than conventional ultrasound imaging.
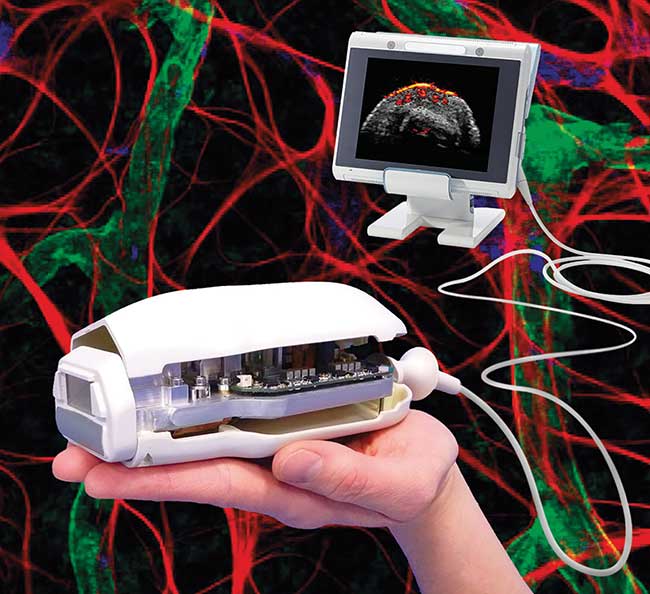
Figure 1. Artist’s impression of a handheld photoacoustic imaging (PAI) medical system integrating a four-wavelength laser diode source. Courtesy of Quantel Laser, Esaote and the University of Twente.
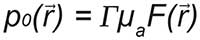
In PAI, light is selectively absorbed according to the spectral properties of potential absorbers. The near-infrared wavelength range shows high potential because of its strong absorption by hemoglobin and its relatively low absorption by water, which enables visualization of blood vessels at a depth of up to a few centimeters. Multiwavelength emission also could enable quantification of blood oxygenation because of the different spectral properties of oxyhemoglobin and deoxyhemoglobin.
However, the introduction of PAI into clinics is hindered by the bulkiness and cost of the laser source. Major advances
in pulsed laser diodes have been made in the last few years, and as a result, their performance today is well-suited for use in photoacoustics. Furthermore, they bring portability and affordability.
PAI will benefit from the numerous advantages that portable imaging systems offer. They can simplify hospital workflows, be shared easily between care centers, help reduce health care costs and offer accessibility to patients who cannot be seen in an office, such as those under home care or in low-resource settings.
Along with the ultrasound receiver, one of the most important PAI components needed to achieve a high penetration depth is the light source. In the photoacoustic mechanism, laser light is absorbed by certain chromophores according to their absorption coefficient µa at the emitted wavelength. This creates a local elevation of temperature, which is then converted into thermal expansion. That local dilatation results in a mechanical wave with a frequency content in the ultrasound regime. The initial pressure generated at locations where optical absorption took place is described by the following equation in which Γ is the Grüneisen parameter that increases as the temperature rises, and F(r) is the local optical fluence:
Because the amplitude of the ultrasound signal recorded by the transducer is proportional to the initial pressure, the PAI device’s sensitivity strongly depends on the local optical fluence received by the absorbers. Because the fluence greatly decreases while passing through human tissues because of absorption and diffusion, the initial peak power of the light source plays a key role in the final performance of the PAI system. It should be higher than tens of kilowatts to achieve images of blood vessels at depth (typically more than 2 cm).
This power level can be achieved with nanosecond pulsed laser systems. Short-pulse duration also enables the laser source to comply with laser safety regulations, as the patient’s skin will have limited exposure to laser light. Also, high-resolution imaging can be made possible by optimizing the pulse duration for the ultrasound transducer’s central frequency and bandwidth. The smallest features can be identified with high-frequency ultrasound transducers, which require very short pulse duration.
Seeking compact devices
Traditional laser sources for PAI mainly have been optical parametric oscillators (OPOs) that can achieve tens of millijoules in pulses shorter than 10 ns at several wavelengths of interest. The limited pulse repetition rate is often an issue for in vivo imaging of tissues in motion as a result of a beating heart. Recent developments in diode-pumped laser systems with pulse emissions at a frequency of 100 to 200 Hz tend to improve the accuracy of image reconstruction. But such laser sources will never be an option in compact and affordable PAI medical devices, preventing the technique from being widely introduced into clinics. Nanosecond Nd:YAG lasers provide a more economical option, but their fixed wavelength (1064 or 532 nm) strongly limits their applications.
Laser diodes are therefore a good candidate because semiconductor sources are highly reliable, compact and low cost. Their high electrical-to-optical efficiency (typically 25 to 30 percent) also enables their integration into handheld devices that require low heat-generation solutions. However, operating high-power laser diodes in a nanosecond pulse regime is not an easy task, especially because kA currents must be handled in very short pulses without generating significant waste heat. Recent developments resulting from different European research programs and led by Quantel Laser, France, now allow introduction of suitable pulsed laser diode sources for PAI.
About five years ago, the first pulsed laser diode demonstrator built for PAI offered around 100-µJ energy in pulses of 150 ns at a wavelength of 808 nm, corresponding to a peak power of 15 kW. Since then, strong research efforts have raised the peak power significantly — as high as 100 kW.
The first step was to increase output energy by using highly efficient semiconductor laser diodes, and then to reduce the pulse duration by minimizing the unwanted self-inductance of contacts and cabling between the diodes and the driver board. A careful optimization of the electrical circuit was required to bring the undesired effect down to an acceptable level.
In 2015, 8-mJ output energy was demonstrated in pulses of 130 ns, corresponding to a peak power of 60 kW. This level of energy can be produced by four small laser diodes integrated into a very compact package. The diodes can be operated either individually or simultaneously and can be built at different wavelengths. Such multiwavelength laser diode sources can be integrated easily into a handheld photoacoustic probe (Figure 1).
Standard wavelengths are 808, 915, 940 and 980 nm. Similar high-output energy can be recorded because of the high efficiency of semiconductor materials. Oxyhemoglobin can be identified with wavelengths in the 9xx-nm range, while deoxyhemoglobin strongly absorbs in the 7xx-nm range. Wavelengths such as 760 nm and 808 nm can be used to visualize reduced hemoglobin, with higher output energies from diodes at 808 nm than at 760 nm because of semiconductor structures (Figure 2).
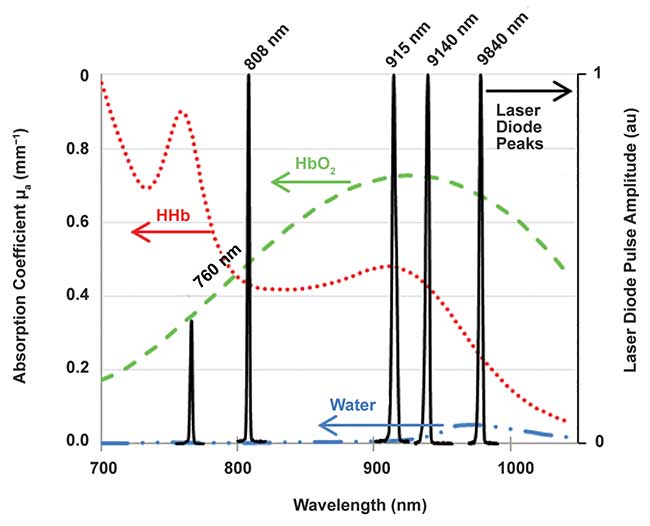
Figure 2. Selected wavelengths for laser diodes and comparison with near-infrared absorption spectra of typical chromophores present in tissue: oxyhemoglobin (HbO2), deoxyhemoglobin (HHb) (cHbO2 = cHHb = 150 g.L-1), and water. (Data extracted from Laufer et al. (2007). Phys Med Biol Vol. 52, pp. 141-168.) Courtesy of Quantel Laser.
More recent advances have produced mJ diodes with pulses as short as 30 ns, and recently as low as 10 ns with state-of-the-art electronic driver boards1,2. All these modules can emit one wavelength at a few kilohertz with an electrical-to-optical efficiency higher than 25 percent. Based on its patented technology, Quantel Laser aims to combine several modules to offer several millijoules in very short pulses and multiwavelength emission.
Demonstration of diode-based PAI in various applications for oncology, rheumatology and the diagnosis of cardiovascular disease has already been successfully performed. Below are a few examples.
Oncology. Extensive research has been undertaken on PAI and photoacoustic tomography (PAT) in oncology. At an early stage of development, a tumor is highly vascularized. Photoacoustics, through identification and quantification of blood vessels, could be valuable for diagnosis of some cancers at an early stage of the disease. The first photoacoustic mammography medical systems, integrating conventional nanosecond lasers, have begun to be introduced into clinical trials for identification of some functional features of breast tumors. These include the tumors’ microvessel distribution pattern and blood oxygenation level.
PAI also could be beneficial in other oncological areas such as thyroid cancer (for detection of tumors) and skin cancer (for identification of malignant melanomas). Human brain tumor imaging with photoacoustics is a real challenge because the skull strongly absorbs and scatters light, as well as attenuates and distorts ultrasound. However, the technique has already been applied to in vivo small animal brain imaging. Research led by Manojit Pramanik from Nanyang Technological University, Singapore, shows compactness and high scan speed in a preclinical photoacoustic tomography system using Quantel’s laser diodes at a frequency of 7 kHz. The experimental device enables 360° scanning with a single-element ultrasound transducer in a few seconds, instead of about five minutes that it would take with low-frequency conventional nanosecond laser sources (Figure 3)3. The team reported that their PAT imaging was done noninvasively (i.e., with the skin and skull intact) and without a contrast agent.
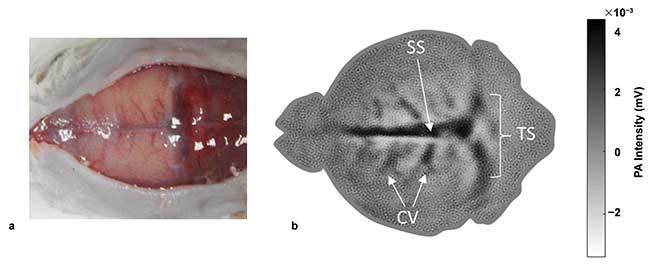
Figure 3. Noninvasive, diode-based photoacoustic tomography images of the vasculature in a 93-g female rat brain. Photograph of the rat brain after removing the scalp (a), in vivo images at a scan time of 30 s. SS: sagittal sinus, TS: transverse sinus, and CV: cerebral veins (b) (See reference 3). Courtesy of Nanyang Technological University.
Rheumatology. Another example of PAI medical devices can be found in the diagnosis of rheumatoid arthritis and the monitoring of finger joint inflammation. Treatments are reported to be more efficient when they are administrated at an early stage of the disease (typically within 1 to 3 months of onset). Early diagnosis and treatment can affect the disease’s course by preventing the development of joint erosions, and in some cases can even lead to remission. At an early stage of the disease, however, diagnosis is based mainly on clinical examination of patients whose main complaint is described as a vague pain, but without the classic symptoms of joint swelling or tenderness. PAI could help in quantifying joint inflammation by visualizing blood vessels, even with only slight signs of inflammation. The Biomedical Photonic Imaging group led by Wiendelt Steenbergen at the University of Twente, the Netherlands, reported the demonstration of a compact, handheld, diode-based, PAI device4. Under the auspices of the European project Fullphase (2011-2016), coordinated by Esaote Europe BV of the Netherlands, the group used the system in a small clinical study (10 patients with rheumatoid arthritis and seven healthy subjects), resulting in a good correlation between photoacoustic signal amplitudes and the degree of inflammation in synovial membranes. The study included comparisons with conventional diagnosis techniques, such as ultrasound power Doppler, and with clinical examination by an experienced rheumatologist5.
Cardiovascular diseases. Last but not least, PAI could have a great impact in the diagnosis of atherosclerosis by identifying whether a matured carotid plaque is potentially vulnerable to rupture. When a rupture occurs, the content of the lesion that enters the blood stream can cause a stroke. Improved diagnosis and risk assessment of plaques after their initial detection could lead to a reduction of these plaque-induced strokes. It also could avoid unnecessary surgeries for patients with a stable plaque.
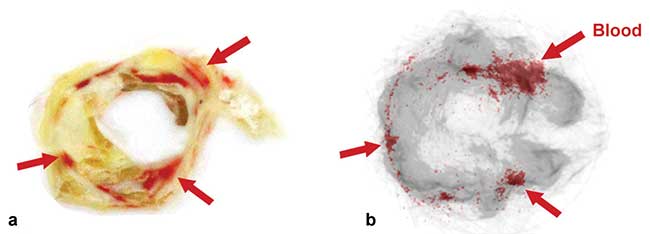
Figure 4. Ex vivo, diode-based photoacoustic imaging of a human plaque. Picture of histology section (a), corresponding cross section in overlaid photoacoustic/ultrasound images (b). The gray color represents the ultrasound signals and the overlaid red colors represent the photoacoustic signals. The red arrows indicate the blood content inside the plaques in the histology picture and the corresponding photoacoustic signals in the overlaid photoacoustic/ultrasound image (See reference 6). Courtesy of the University of Eindhoven.
A demonstration of ex vivo imaging to identify intraplaque hemorrhages in carotid plaques using photoacoustics has been performed by The Eindhoven University of Technology, the Netherlands. The research group in the Department of Biomedical Engineering, led by Richard Lopata, recently published their study in which a good correlation was found between hemorrhage locations visualized from histology sections of the plaque and the photoacoustic signal from a laser diode at 808 nm (Figure 4)6. These exciting results are the first step toward in vivo PAI imaging, which will be the next step for 10 European partners, including Quantel Laser, through a Horizon 2020 project called CVENT (2016-2019).
Meet the authors
Celine Canal is in charge of research and development of ultrashort pulsed laser diode sources at Quantel Laser. She also manages a work package in European programs (Fullphase, CVENT) for development of a laser diode source for integration in a handheld device for medical diagnosis; email: [email protected]. Andreas Kohl has worked on high-power diode lasers and laser systems since 2004, first at Thales and later at Quantel Laser, where he has held several positions, including project manager for major defense and space programs; head of research and development for laser diodes; and today as head of operations for laser diodes; email: [email protected].
Acknowledgments
The CVENT project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 731771. http://cvent-2020.eu/.
References
1. Canal et al. (2016). Portable multiwavelength laser diode source for handheld photoacoustic devices. Proc SPIE, 9887, 98872B.
2. Canal et al. (2017). Novel short-pulse laser diode source for high-resolution 3D flash LIDAR. Proc SPIE, 10332, 103320B.
3. Upputuri et al. (2017). A high-performance compact photoacoustic tomography system for in vivo small-animal brain imaging. J Vis Exp (124), e55811.
4. Daoudi et al. (2014). Handheld probe integrating laser diode and ultrasound transducer array for ultrasound/photoacoustic dual modality imaging. Opt Express, Vol. 22, Issue 21, pp. 26365-74.
5. http://www.fullphase-fp7.eu/.
6. Arabul et al. (2017). Toward the detection of intraplaque hemorrhage in carotid artery lesions using photoacoustic imaging. J Biomed Opt, Vol. 22, Issue 4, 041010.