Finding the right match of sensitizer and wavelength helps propel treatments.
Dr. Krystyna Konopka, University of the Pacific, San Francisco, and Dr. Tomasz Goslinski, University of Medical Sciences, Poznan, Poland
Photodynamic therapy (PDT) involves the use of a photosensitizer that is activated by illumination in the presence of oxygen. The exposure of the photosensitizer to light results in the formation of toxic oxygen species, thereby causing localized photodamage and cell death. Applications of the technique in dentistry may include photodynamic diagnosis of malignant transformation of oral lesions, treatment of premalignant and malignant oral lesions, and chemotherapy (PACT) of bacterial and fungal infections. Photodynamic therapy already has shown potential in the treatment of oral leukoplakia, oral lichen planus and squamous cell carcinoma of the tongue and lip.1
In photodynamic therapy, a photosensitizer or its metabolic precursor is administered to the patient. An overview of the photodynamic reaction is provided in Figure 1. Photodynamic therapy requires activation of the photosensitizer via exposure to low-power visible light at a specific wavelength. Human tissue transmits red light efficiently, and the longer activation wavelength of the photosensitizer results in deeper light penetration. Consequently, most photosensitizers are activated by light between 630 and 700 nm, corresponding to a penetration depth of 0.5 cm (at 630 nm) to 1.5 cm (at ~700 nm). The total light dose, the dose rate and the depth of destruction vary with each tissue that is treated and with each of the available photosensitizers.2
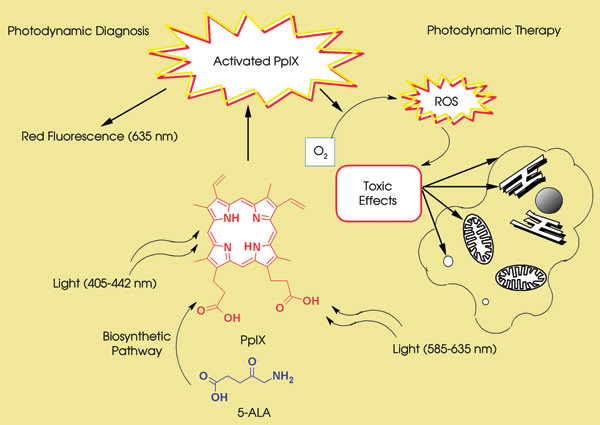
Figure 1. Light of an appropriate energy (that is, with a wavelength at the absorption maximum) is absorbed by protoporphyrin IX (PpIX), which undergoes a transition from a low-energy ground state to the excited singlet state. In photodynamic therapy, the activated photosensitizer interacts with oxygen to produce singlet oxygen and other radical species that cause a toxic effect in tumor cells or microorganisms. In photodynamic diagnosis, the illumination of PpIX (irradiated at a lower wavelength than in photodynamic therapy) leads to the emission of red fluorescence. ROS = reactive oxygen species; 5-ALA = 5-aminolevulinic acid.
Easy to handle, portable and cost-effective diode laser systems predominantly are used. For treatment of larger areas, noncoherent light sources such as tungsten filament, quartz halogen, xenon arc, metal halide and phosphor-coated so?dium lamps are used. Recently, LEDs have been applied in photodynamic therapy because they are small, lightweight, highly flexible and less expensive than typical light sources.
Sources used for light delivery depend upon the location and morphology of the lesion, but typically they are fiber optic catheters terminated with cylindrical diffusers or lenses for flat-field applications. Fiber tips can be made into various shapes, allowing for diffusion in all directions or for tighter focus.
An ideal photosensitizer should display local toxicity only after illumination. The majority of the sensitizers used clinically are phenothiazine dyes or porphyrin-chlorin-phthalocyanine platforms. Photofrin (dihematoporphyrin ether), the most extensively studied and clinically used photosensitizer, and hematoporphyrin derivatives are referred to as first-generation sensitizers. Second-generation photosensitizers include 5-aminolevulin-ic acid (ALA), benzoporphyrin deriva-tive, lutetium texaphyrin, temoporfin (mTHPC), tinethyletiopurpurin and talaporfin sodium. Foscan (temoporfin), the most potent second-generation photosensitizer, has been found to be 100 times more active than Photofrin in animal studies.3 ALA, a precursor of the fluorescent photosensitizer protoporphyrin IX (PpIX), can be administered systemically or applied topically to the oral mucosa and the skin.
Only four photosensitizers are commercially available: Photofrin, ALA, Visudyne (a benzoporphyrin derivative, verteporfin) and Foscan. The FDA has approved the first three, whereas all four are used in Europe. Two ALA preparations, Metvix (PhotoCure ASA, Oslo, Norway) and Levulan Kerastic (Dusa Pharmaceuticals, Wilmington, Mass.), have been approved by the European Agency for the Evaluation of Medicinal Products and by the FDA, respectively, for the treatment of nonhyperkeratotic actinic keratoses of the face and scalp. PDT has not been approved by the FDA for use in dentistry. In clinical trials, all patients are treated in accordance with the FDA and local Institutional Review Board approval.
Diagnosis of oral lesions
Accounting for 96 percent of all oral cancers, squamous cell carcinoma is usually preceded by dysplasia seen as adherent white lesions on the oral mucosa (leukoplakia). The prognosis of patients with oral cancer might be improved greatly by early diagnosis. Currently, a definitive diagnosis can be obtained only via random tissue biopsy, which is subject to sampling error, patient discomfort and scarring. Other screening methods do not provide more conclusive data. Toluidine blue staining is sensitive but not specific and is not approved by the FDA, and cytological scraping of lesions usually produces poor cell yields and lacks definitive biomarkers for diagnosis.
A relatively new approach in the diagnosis of oral lesions is topical application of ALA. In ALA-mediated photodynamic diagnosis, an intracellular accumulation of PpIX increases tissue fluorescence. Subsequent illumination leads to red fluorescence of the lesion caused by endogenous and ALA-induced PpIX. The difference in the fluorescence ratio between normal and premalignant/malignant tissue facilitates the distinction between malignant and nonmalignant lesions. Applications of fluorescence in diagnosis are provided in Figure 2.
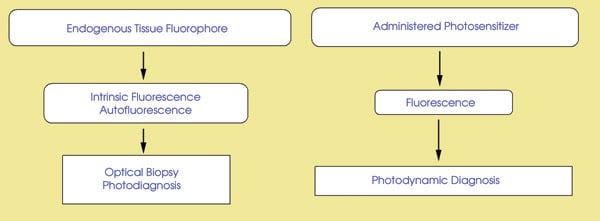
Figure 2. Optical biopsy, or photodiagnosis, employs the fact that carcinogenesis causes molecular and structural changes in tissue. These changes are seen as the differences in the autofluorescence between benign and premalignant/malignant tissue. In photodynamic diagnosis, tissue fluorescence is induced by illumination of the administered photosensitizer.
Compared with nonoptical techniques, ALA-based photodynamic diagnosis offers potential advantages such as a noninvasive diagnosis, in situ monitoring, cost-effectiveness and better tolerance than surgical biopsy for the patient. Because of the limited depth of topical ALA and the limited light penetration of tissue at 635 nm, the use of ALA is restricted to superficial lesions (1 to 2 mm deep).
A. Sharwani of the London-based Eastman Dental Institute for Oral Healthcare Sciences and colleagues examined 71 patients who exhibited clinically suspicious oral leukoplakia.4 Three hours prior to examination, the patients rinsed their mouths with a 0.4-percent solution of ALA for 15 min. This relatively short contact with ALA is advantageous for diagnosis because the fluorescence intensity in malignant tissue decreases rapidly following ALA application.
Illumination was performed by a xenon-arc lamp at 425 nm. An optical endoscope was used both for illumination and for detection of tissue fluorescence. PpIX accumulated in the premalignant/malignant and normal tissue was excited via an endoscope, and the fluorescence image was obtained using a single-chip CCD color camera.
PpIX fluorescence and autofluorescence were imaged by the red and green channels, respectively. The results of the fluorescence spectroscopy were compared with histopathology. Dysplastic lesions have significantly higher red fluorescence than benign oral lesions without changes in green autofluorescence.
In clinical trials, a combination of autofluorescence and PpIX fluorescence allows a better demarcation between malignant and healthy tissue. To assess the feasibility of fluorescence-guided tumor resection and the potential outcomes of topical ALA-based photodynamic therapy, it is essential to determine the penetration depth and tissue distribution of PpIX fluorescence.5
Light-induced fluorescence using topical Photofrin also can provide a sensitive noninvasive method for the early diagnosis of oral cancer. Twenty patients with suspicious oral lesions received Photofrin solution (2.5 mg/ml) topically. After three hours, they underwent illumination (λex = 370 to 450 nm). Eighty mucosal biopsy samples obtained from four different sites for each patient were examined for histopathologic confirmation. The specificity of the neoplastic tissue, evaluated using the red, green, and blue and gray-scale modes, was 95.65 percent in the macroscopic study and 97.5 percent in the microscopic study.
Although some visible red fluorescence was detected in the surrounding tissue, the difference between healthy tissue and the lesions as a group was statistically significant.6
Oral leukoplakia and oral verrucous hyperplasia are common premalignant lesions that may transform into squamous cell or verrucous carcinoma. Topical ALA-based photodynamic therapy has been used to treat premalignant and malignant lesions in the oral cavity (Figure 3). Photodynamic therapy of the oral mucosa causes superficial necrosis, leaving little scarring and no cumulative toxicity. ALA-based photodynamic therapy appears to be an effective treatment for oral leukoplakia.1 This may be attributed to its low invasiveness, good tolerance, excellent cosmetic effects, ability to treat multifocal lesions and low risk of toxicity after repeated use. Variations observed in the treatment findings could result from various ALA preparations, the number of ALA applications, the incubation period (1.5 to 5 h), the light source (laser or LED), the illumination protocol (continuous or fractionated) and the number of treatments.
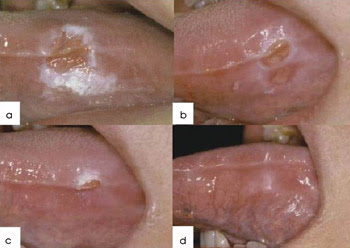
Figure 3. Shown is a leukoplakia lesion on the tongue, treated topically with ALA followed by LED irradiation at 100 J/cm2. (a) Before treatment; (b) one week after the first treatment; (c) one week after the second treatment; (d) one week after the third treatment. The leukoplakia improved gradually and disappeared finally after three treatments. Reprinted with permission from J.C. Tsai et al, “Photodynamic therapy of oral dysplasia with topical 5-aminolevulinic acid and light-emitting diode array,” Lasers in Surgery and Medicine, January 2004, pp. 18-24.
The oral cavity is colonized by relatively specific and highly interrelated microorganisms, including aerobic and anaerobic Gram-positive and -negative bacteria, fungi, mycoplasma, protozoa and viruses. Dental plaque is a complex aggregation of microorganisms found on the tooth surface in the form of a biofilm; that is, the organisms are embedded in an extracellular polymeric matrix. Biofilm-associated bacteria have increased resistance to antibiotics, to environmental stresses and to the immune defense mechanisms of their host.
Two of the most common bacterial diseases afflicting humans — dental caries and periodontal diseases — result from a buildup of plaque biofilms on the teeth and soft tissues of the mouth. The limited access of topical agents into the plaque and the development of antibiotic resistance have stimulated the search for new strategies to control plaque and to treat caries, gingivitis and periodontal disease. PACT is equally effective against antibiotic-resistant and -susceptible bacteria, and repeated photosensitization has not induced the selection of resistant strains.7
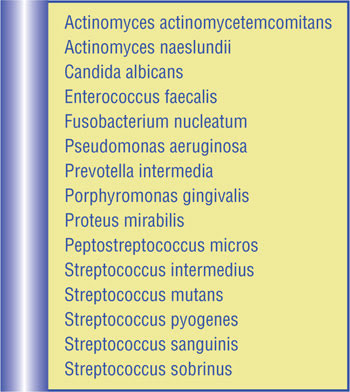
Table 1. Bacteria and fungi that respond to photodynamic antimicrobial chemotherapy (PACT).
Because the antimicrobial activity of photosensitizers is mediated by singlet oxygen, PACT has a direct effect on extracellular molecules, and the polysaccharides of an extracellular polymeric matrix also are susceptible to photodamage. This dual activity, not displayed by antibiotics, represents a significant advantage of PACT.
The activity of PACT against homogeneous and mixed Gram-positive and -negative bacterial and fungal oral biofilms (Table 1) has been reported for a range of photosensitizers (Table 2). In addition to the treatment for periodontitis, PACT for peri-implantitis, endodontic treatment and caries also has come into focus.
Biofilms of Streptococcus intermedius, prepared in artificial root canals and extracted human teeth, have been subjected to PACT using toluidine blue O, a laser diode device emitting at 633 nm and an endoscopic tip that allowed light to be transmitted down to the tooth’s apex. Photoactivated disinfection significantly reduced the number of bacteria in both types of root canals.
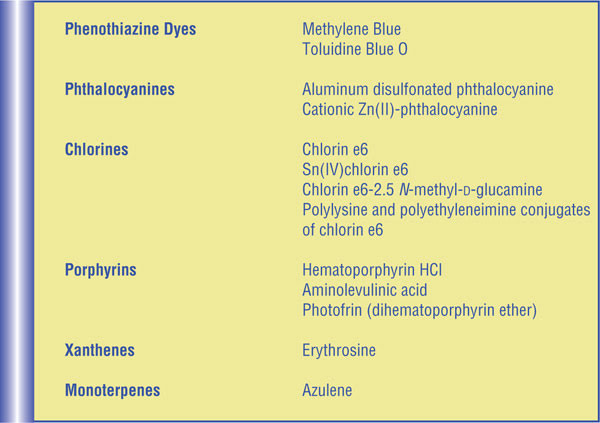
Table 2. Photosensitizers applied in PACT.
In other tests, methylene blue in combination with 665-nm irradiation eliminated 97 percent of Enterococcus faecalis biofilm bacteria in root canals of extracted teeth. Biofilms of Proteus mirabilis and Pseudomonas aeruginosa, prepared in extracted human teeth, were treated with a conjugate of polyethyleneimine with chlorin e6 followed by illumination with a 660-nm diode laser. PACT alone reduced the bioluminescence by 95 percent, while the combination of standard endodontic treatment with the photodynamic technique reduced bioluminescence by more than 98 percent. Electron microscopy revealed complete eradication of bacteria in biofilms of Actinobacillus actinomy?cetemcomitans, Porphyromonas gingivalis or Prevotella intermedia prepared on implant surfaces treated with toluidine blue O and irradiated at 905 nm.1
Oropharyngeal candidiasis — caused by Candida albicans and related species — is a widespread opportunistic infection in immunocompromised patients, such as HIV-infected individuals. In addition, Candida-associated denture stomatitis is a common disease in denture wearers. The ability of C. albicans to form biofilms on mucosal surfaces and on prosthetic devices contributes to recurrent infections and to the failure of antifungal therapy.
The increasing resistance of C. albicans to antifungal agents has stimulated an interest in photodynamic treatments. Similarly to other yeasts, C. albicans is more difficult to kill by PACT than are Gram-positive bacteria. Recently, Ryan F. Donnelly and his colleagues at Queen’s University Belfast in the UK reported on mucoadhesive patches containing toluidine blue O as a potential delivery system in oral candidiasis.8
Future directions
The studies summarized in this review indicate that photodynamic techniques have considerable potential in dentistry. Successful photodynamic treatment is, however, limited by the lack of accurate dosimetry and suitable illumination devices, as well as by insufficiently defined treatment parameters. New photosensitizers and more efficient light-delivery systems, along with animal studies, are required to establish the optimum treatment parameters before the technique can proceed to clinical trials.
Although the photoinduced antibacterial properties of methylene blue and of toluidine blue O have been known for a long time, the introduction and adoption of antibiotics have delayed the progress of PACT. Increasing bacterial resistance to antibiotics requires the development of alternative treatments.
PACT appears most efficient for localized and superficial infections. Thus, infections in the oral cavity — such as mucosal and endodontic infections, periodontal diseases, caries and peri-implantitis — are potential targets. PACT will not replace antimicrobial chemotherapy, but the photodynamic approach may improve treatment of oral infections, speeding up treatment and lowering its cost.
Meet the authors
Krystyna Konopka is a professor in the microbiology department at the University of the Pacific’s Arthur A. Dugoni School of Dentistry in San Francisco; e-mail: [email protected]. Tomasz Goslinski is an assistant professor in the department of chemical technology of drugs at the University of Medical Sciences in Poznan, Poland; e-mail: [email protected].
References
1. K. Konopka and T. Goslinski (August 2007). Photodynamic therapy in dentistry. J Dent Res, pp. 694-707.
2. A.C. Kübler (May 2005). Photodynamic therapy. Med Laser Appl, pp. 37-45.
3. R.R. Allison et al (January 2004). Photosensitizers in clinical PDT. Photodiagn Photodyn Ther, pp. 27-42.
4. A. Sharwani et al (January 2006). Fluorescence spectroscopy combined with 5-aminolevulinic acid-induced protoporphyrin IX fluorescence in detecting oral premalignancy. J Photochem Photobiol B, pp. 27-33.
5. A. Leunig et al (January 2001). Fluorescence staining of oral cancer using a topical application of 5-aminolevulinic acid: fluorescence microscopic studies. J Photochem Photobiol B, pp. 44-49.
6. C.-J. Chang and P. Wilder-Smith (June 2005). Topical application of Photofrin for photodynamic diagnosis of oral neoplasms. Plast Reconstr Surg, pp. 1877-1886.
7. M. Wainwright and K.B. Crossley (March 2004). Photosensitizing agents — circumventing resistance and breaking down biofilms: a review. Int Biodeteriorat Biodegrad, pp. 119-126.
8. R.F. Donnelly et al (January 2007). Potential of photodynamic therapy in treatment of fungal infections of the mouth. Design and characterization of a mucoadhesive patch containing toluidine blue O. J Photochem Photobiol B, pp. 59-69.