Researchers at Skoltech are a step closer to a working optoacoustic endoscopic probe — a device that could slip inside a blood vessel and analyze atherosclerotic plaques by shining laser light on them and making them vibrate like a speaker membrane. This effect would cause the plaques to betray their chemical composition with an ultrasound signature. The method, if it can be achieved, would prove useful for robotic microsurgeries and medical diagnostic procedures.
Unlike a CT scan, optoacoustic imaging does not use x-rays or other harmful radiation. It instead relies on visible light and sound signals. Optoacoustics expose biological tissue to pulses of laser light at a wavelength absorbed by some medically significant molecule — hemoglobin or collagen, for example. Each pulse heats the molecules of interest (or biomarkers), causing expansion and then contraction in the moments before the next pulse arrives.
The periodic oscillation effectively turns the markers into miniature speakers that reveal their locations by emitting ultrasound, which can be picked up by a sensitive microphone. Advantages of optoacoustic diagnostics go beyond radiation safety; the technique enables the ability to target specific biomarkers by varying the wavelength of the laser used to excite acoustic waves. Additionally, ultrasound experiences fairly low attenuation in biological tissues, meaning that it can travel greater distances before the signals dies down, compared to light, affording a deeper look into the body.
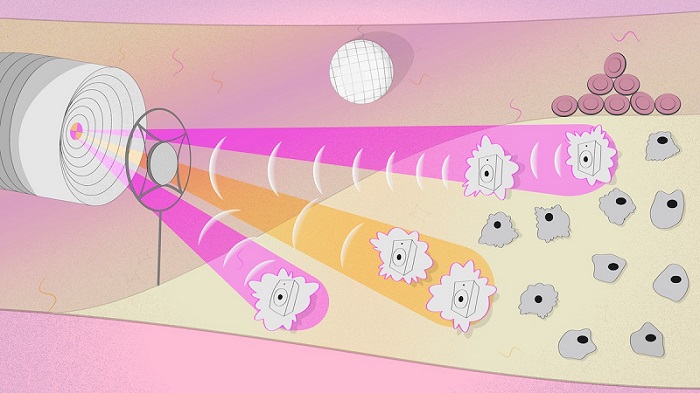
An artist’s impression of an optoacoustic probe. The probe comes into the blood vessel to inspect the composition of an atherosclerotic plaque. The device exposes the constituent cells to light at various wavelengths so they just can’t stand still and picks up the resulting vibrations with a microphone. Courtesy of Pavel Odinev/Skoltech.
Dmitry Gorin, the study’s principal researcher and a professor in the Center for Photonic Science and Engineering at Skoltech, said that existing optoacoustic diagnostic systems are bulky and not intended to be introduced into the body. “Sometimes a laser just cannot penetrate deep enough, so you have to put a probe inside the body to get a closer look at the insides of a blood vessel or the bladder, for example,” Gorin said. “This would be useful for inspecting atherosclerotic plaques or possibly even doing microsurgery on them. The probe has to be really thin and should ideally not have any wires.”
To this end, the researchers are elaborating a setup originally proposed by a team of their colleagues in England. The probe in question is made of an optical fiber that transmits laser pulses and carries a membrane. The membrane serves as a tiny microphone on its tip. In the system, pulses from one laser are intended to arrive at the tip of the probe, pass freely through the membrane, and excite the biomarker. Once it emits acoustic waves, they are picked up by the membrane. A second laser then reads out the signal from the membrane.
“We used a 100-nm film of carbon nanotubes as the microphone membrane. To enable signal readout from the membrane via laser light, we deposited a so-called Bragg mirror of titanium dioxide and silicon dioxide on the nanotube layer,” said study first author Nikita Kaydanov. “As the mirror oscillates along with the membrane, this modulates the laser signal, enabling readout.”
The Skoltech researchers also incorporated a hollow-core microstructured waveguide — an optical fiber that has an air cavity running along its entire length at the center. The benefit of using such fiber is in its ability to transmit light in the otherwise unavailable mid-infrared range. This can be used to target additional biomarkers such as carbohydrates, lipids, and proteins, and including those needed to distinguish between atherosclerotic plaques that are relatively harmless and those that require medical attention.
In the study, the team also acquired valuable data on how the laser heats up a mirror component in the system and how this affects its refraction index. This information is essential for correct signal interpretation, the researchers said.
“Our experiment also demonstrated signal readout with a laser from the oscillating mirror-coated membrane,” Gorin said. “However, what moved the membrane in our case was not actually the sound wave emitted by biomarkers but the initial laser pulse that lost some of the energy in passing through the membrane.”
According to the researchers, knowledge of how the signal readout works and of the system’s inherent “background” signal will enable them to try to pick up actual ultrasound waves from the environment to show that the device can function.
The research was published in ACS Photonics (www.doi.org/10.1021/acsphotonics.1c01311).