Tens of millions of people around the world suffer from corneal diseases, with only a small fraction eligible for corneal transplantation. In a recent study, researchers at the University of Ottawa showed that biomimetic materials activated with low-energy blue light can reshape and thicken damaged corneal tissue to promote healing and recovery. The research results could provide a safe way to treat corneal thinning, as well as a practical alternative to corneal transplantation.
Further, the dosage of pulsed blue light needed to activate the biomaterial is minimal, which mitigates the possibility of cytotoxic effects from the light.
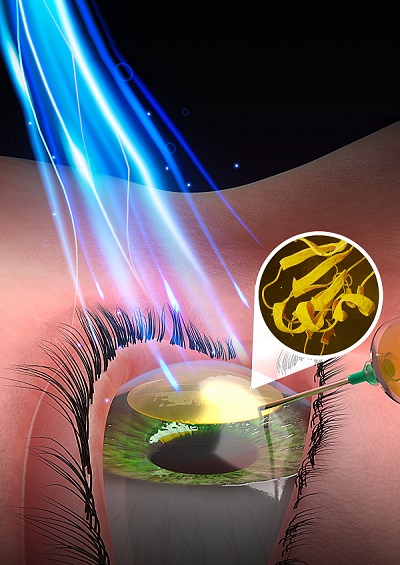
An injectable biomaterial activated by pulses of low-energy blue light has tremendous potential for on-the-spot repair to the domed outer layer of the eye, University of Ottawa researchers and their collaborators have revealed. Courtesy of Faculty of Medicine, University of Ottawa.
The biomaterial is injected within the corneal tissue after a tiny pocket is surgically created. The injectable biomaterial, which is in the form of a viscous liquid, is made from short peptides and glycosaminoglycans that assemble into a hydrogel when irradiated with low-energy blue light. The hydrogel hardens and forms a tissue-like 3D structure with properties similar to those found in pig corneas. The use of low-energy pulsed light irradiation allows the researchers to safely use photocuring to photo-crosslink the biomimetic materials designed for injection into thinning corneas.
Data showed that the materials used to obtain experimental test results could remain in an animal model for several weeks. As a result, professor Emilio Alarcon and the other researchers anticipate that the material will remain stable and be nontoxic in human corneas.
In their study, the researchers observed that the way the light was delivered affected the formation of the hydrogel. Pulsed irradiation allowed for better recovery of the oxygen levels within the hydrogel, compared to a continuous dosage of light. Pulsing the light for 2.5 s on, 2.5 s off produced optimal results.
To keep the light dosage under standard safety values, the researchers selected a low in vivo radiance dosage of 8.5 mW cm−2 for 10 min of pulsed light, which is equivalent to only 5 min of light exposure. This radiance level is below the category of low risk when direct blue light is exposed to the eye for up to 166 min. The researchers performed in vivo experiments for light toxicity on animal models to verify the safety of their light irradiation regime.

In vivo experiments using a rat model indicated that the light-activated hydrogel could thicken corneas without side effects. The researchers also successfully tested the technology in an ex vivo pig cornea model.

Emilio Alarcon, an associate professor at the University of Ottawa’s Faculty of Medicine and researcher at the BioEngineering and Therapeutic Solutions (BEaTS) group at the University of Ottawa Heart Institute. Courtesy of Faculty of Medicine, University of Ottawa.
According to Alarcon, the researchers developed the technology to be clinically translatable; all components must be designed to be manufacturable following strict standards for sterility. In clinical conditions, reducing the amount of light delivered to the eye will translate into a faster and safer procedure. It will shorten the period during which eye movement must be minimized to ensure stability of the injected biomaterial volume and shape until it turns into a soft hydrogel. Good control of the corneal front surface curvature is of primary importance for adequate refraction of the light within the eye.
Although testing in large animal models will be necessary prior to clinical human trials, the researchers have begun the patent application process for the technology.
The research was published in Advanced Functional Materials (www.doi.org/10.1002/adfm.202302721).