
Lasers Improve Phototherapy-Drug Delivery Platform
Photoimmunotherapy targets cancer cells with microscopic, nano-engineered cancer drugs that are light-activated at the lesion site. Although the technology is increasingly used to treat metastatic cancer, tools to improve the effectiveness of photoimmunotherapy in gynecologic oncology have been lacking. Responses to treatment vary from person to person, and no method has existed to readily monitor whether the drugs are delivered effectively or have the desired therapeutic effect.
Researchers from the University of Maryland (UMD), in collaboration with medical laser manufacturer Modulight, demonstrated that the efficacy, safety, and consistency of photoimmunotherapy can be improved by integrating targeted, light-based techniques for drug delivery with laser-assisted endoscopy and fluorescence-guided treatment planning.
The researchers designed a drug delivery system using targeted, photo-activable, multi-agent liposomes (TPMAL). TPMAL consists of chemotherapy drugs that are labeled with fluorescent markers. It improves therapeutic delivery and monitors the growth of metastases in difficult-to-treat locations within the body.
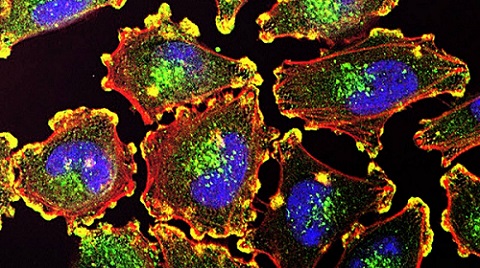
UMD researchers have successfully combined three photoimmunotherapy technologies to help prevent the spread and return of metastatic cancer, while minimizing side effects of treatment. Courtesy of the National Institutes of Health.
A laser-assisted endoscopic camera created by Modulight captures and uploads information from TPMAL to Modulight Cloud, a cloud services platform. Modulight Cloud analyzes the multispectral fluorescence emission from TPMAL in real time to enable fluorescence-guided drug delivery and fluorescence-guided light dosimetry. The real-time connectivity enables simultaneous treatment monitoring, remote protocol development, and rapid transfer and viewing of data.
The data acquired by the camera can be used to customize fluorescence-guided therapy. Doctors can use the data to determine, in real time, how well the drug-carrying liposomes are reaching and delivering treatment to metastatic cancer sites. They can also use the data to calculate the precise amount of laser light needed during photoimmunotherapy to minimize tissue damage.
The optimal accumulation of TPMAL in tumors can occur at different times for different patients. Fluorescence-guided drug delivery identifies the time when the TPMAL fluorescence signal is near peak levels in tumors, thereby informing the initiation of photoimmunotherapy for the best outcome.
The TPMAL levels in tumors can vary among patients. Fluorescence-guided light dosimetry monitors the photobleaching of photosensitizers during photoimmunotherapy, so that the light dose can be adjusted accordingly, in real time, to improve the consistency of treatment effects.
“Patients undergoing cancer treatment exhibit varying tolerances and individualized responses,” said UMD professor Huang Chiao Huang. “Through continuous monitoring of their progress, we can promptly determine if treatment adjustments are needed while they are actively receiving care. There is no need to postpone decisions until the next scheduled session.”
The researchers demonstrated their approach in mouse models with peritoneal carcinomatosis, a type of cancer that can be caused by metastatic ovarian cancer. They observed a fourteenfold improvement in drug delivery to metastatic tumors. The information captured by the endoscopic camera prompted fluorescence-guided light dosimetry in over 50% of the mice. By combining TPMAL, laser-assisted imaging, and fluorescence-guided intervention, the researchers achieved a more homogeneous response to treatment in the mice and improved tumor control without causing side effects.
Although nearly half of the women with advanced ovarian cancer achieve complete remission after surgery and chemotherapy, many patients will relapse due largely to residual submillimeter lesions. These residual micro-metastases are difficult to detect and often develop resistance to standard treatments. New approaches are needed to address these drug-resistant micro-metastases.
The UMD-Modulight study shows that a combination of targeted photomedicine drug delivery, imaging, and monitoring of treatment responses can help prevent the return and spread of cancer while minimizing the side effects of treatment. Together, the three techniques can give doctors the ability to make immediate adjustments in treatment to achieve better outcomes.
“This approach ensures that the treatment remains both effective and uniform,” Huang said. “This process is repeated as necessary for each patient, resulting in a personalized dosage tailored to maximize treatment effectiveness within a single session.”
The team is now working to establish a comprehensive panel of biomarkers that would allow doctors to promptly determine the optimal dosage for each patient during a treatment session.
“The goal is to minimize the number of treatment cycles required while minimizing burden on the patient’s body, in contrast to conventional treatment approaches,” Huang said.
The research was published in Science Advances (www.doi.org/10.1126/sciadv.adi3441).
/Buyers_Guide/Modulight_Inc/c9763
/Buyers_Guide/Modulight_USA_Inc/c9764