
Artificial Cornea is in Sight
STANFORD, Calif., Sept. 20, 2006 -- A novel biomimetic material -- a hydrogel or polymer that holds a lot of water -- is finding its way into artificial corneas and may promise a new view for at least 10 million people worldwide who are blind due to damaged or diseased corneas or many millions more who are nearsighted or farsighted due to misshapen corneas.
The research was presented on Sept. 11 in San Francisco at the annual meeting of the American Chemical Society by Stanford University chemical engineer Curtis W. Frank.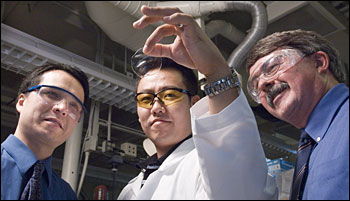
Engineers and doctors partnered to create a biomimetic hydrogel for use in artificial corneas. Stanford University medical student David Myung holds a sample of the hydrogel, a product of an interdisciplinary collaboration led by ophthalmology assistant professor Christopher Ta (left) and chemical engineering professor Curtis Frank (right). (Photo: L.A. Cicero)
Called Duoptix, the material can swell to a water content of 80 percent -- about the same as biological tissues. It's made of two interwoven networks of hydrogels. One network, made of polyethylene glycol molecules, resists the accumulation of surface proteins and inflammation. The other network is made of molecules of polyacrylic acid, a relative of the superabsorbent material in diapers.
"Think of a fishnet, but think of a 3-D fishnet," said Frank, the W. M. Keck Senior Professor and a professor, by courtesy, of chemistry and of materials science and engineering. "It's a strong, stretchy material." That makes it able to survive suturing during surgery. The biocompatible hydrogel is transparent and permeable to nutrients, including glucose, the cornea's favorite food.
Collaborators on the hydrogel work that Frank presented at the chemists' meeting are Marianne E. Harmon with GE Corporate Research Lab in Schenectady, N.Y.; Dirk Kucklung, an assistant professor at the Institute for Polymer Science in Dresden, Germany; Wolfgang Knoll, director of the Max Planck Institute for Polymer Research in Mainz, Germany; and David Myung, a medical student jointly working on a doctorate in chemical engineering in Frank's lab. 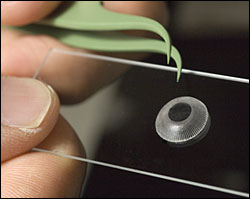
The artificial cornea is made of a dual-network hydrogel with a clear center and peripheral pores. Cells infiltrate the pores and secrete collagen, which integrates the artificial cornea into the surrounding natural tissue. (Photo: L.A. Cicero)
Myung's project, funded by Stanford's Bio-X interdisciplinary biosciences program, was to design, fabricate and characterize a bioengineered cornea based on the dual-network hydrogel. The result was a disc with a clear center and tiny pores populating the periphery. Myung calls the pores engineered into his artificial cornea the "homes" he built for cells that need to infiltrate the artificial lens and integrate it with surrounding natural tissue.
"If you build it, they will come," Myung said. "The cells move in, and they bring furniture too -- meaning the collagen they secrete. They even 'remodel.'" Collagen binds to the edge of the synthetic disc and forms a junction between natural and synthetic tissues. Then a clear layer of epithelial cells grows over the disc.
Stanford's program to develop an artificial cornea is "broadly interdisciplinary," Frank said. Christopher Ta, an assistant professor of ophthalmology and ophthalmology residency director at the Stanford University Medical Center, leads the effort with Frank. Ta said scientists have tried to develop artificial corneas for half a century, but prototypes were not well tolerated. Infections developed around implants or eyes extruded implants.
A few years ago, in a pilot study for a Bio-X grant to show proof of concept, Ta began to test the hydrogel in assays to make sure it was not toxic to cells. Soon other experts joined the effort. Jaan Noolandi in the ophthalmology department managed projects, worked with potential sponsors and provided insight into polymer physics. Nabeel Farooqui, also in ophthalmology, developed histology procedures.
Won-Gun Koh, a former postdoctoral fellow in chemical engineering, first synthesized the polymer that Myung ultimately developed. Qi Liao, a chemical engineering graduate student, contributed to a general understanding of the hydrogels. Jennifer Cochran, assistant professor in the bioengineering department, is investigating how to maximize epithelial adhesion to the material. Michael Carrasco, a peptide chemist at Santa Clara University, consulted about surface modifications for cellular adhesion.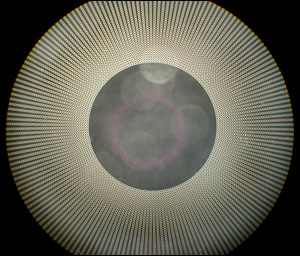
This pattern, created with photolithography, is used to make the artificial cornea. (Image: David Myung) | |
The researchers are now testing the material for biocompatibility in animal models. Animals have tolerated artificial corneas with no problems in trials as long as eight weeks, Ta said, and the material remains perfectly clear. Longer trials are a next step.
The current source of tissue for corneal transplants is cadavers. Donor tissue has problems, Ta notes, including a rejection rate of about 20 percent and a period for visual recovery of six months to a year. "You get a more predictable shape with an artificial cornea," Ta said.
"In many countries, tissue availability is a problem," he said. "If the tissue is artificial, we don't have to rely on donor tissue." The high prevalence of laser-assisted in situ keratomileusis, or LASIK, eye surgery may contribute to the shortage of donor tissue in developed nations, he notes, as this surgery disqualifies donation. A tissue-engineered artificial cornea could lessen or eliminate the need for donor tissue.
At least a dozen groups worldwide are working to develop artificial corneas, Myung said. "Only two or three are on the market, but they are only used in last-ditch efforts (when transplants are rejected)." Stanford's artificial cornea is "the most biomimetic," he said, with a water concentration and mechanical properties that rival those of the natural cornea.
"The dream would be to have a corneal replacement that's sterilized and dehydrated and sent off to the hospital or battlefield, and rehydrated," Frank said.
Other ocular applications of the hydrogel could include more comfortable extended-wear contact lenses.
Inlays and onlays are also possible. The cornea contains layers -- a top layer of protective epithelial cells, a middle layer called stroma that provides the collagen matrix that gives the cornea its shape and an innermost endothelial layer. With onlays, some of the epithelial layer can be scraped away and replaced with a hydrogel contact lens. The lens becomes biointegrated when clear epithelial cells grow over the top of the lens. Inlays, on the other hand, are implanted within the stroma.
Inlays and onlays offer advantages over LASIK surgery, which works but isn't reversible, Myung says. He envisions implantable contact lenses that can be replaced if the prescription changes.
Hydrogel lenses may even make their way deeper into the eye as replacements for inner-eye lenses damaged by cataracts.
The researchers have filed four patents for ocular applications of the hydrogel. Funding for the project came from Stanford's interdisciplinary Bio-X program; Santa Clara, Calif.-based VISX, manufacturer of a laser used in LASIK eye surgery; Stanford's Office of Technology Licensing; Stanford Medical Scholars Program; and the nonprofit organization Fight for Sight.
For more information, visit: http://news-service.stanford.edu
Published: September 2006